1
INTRODUCTION
The Physician Assistant Student Handbook has been created as a reference for students enrolled in the Utah Valley University Physician Assistant Program (“program” or “PA program”) and others seeking information about the program. These policies and procedures apply to all PA students. This handbook also serves to demonstrate Utah Valley University’s (UVU) compliance with the accreditation standards established by the ARC-PA.
This handbook provides an overview of all aspects of the program. It contains policies and procedures for academic and professional standards, and progress throughout the program. It also contains university wide policies and information about resources available through UVU. This handbook was designed to supplement existing university policies and procedures that relate to the program. All students are strongly encouraged to become familiar with this handbook, other program policies, and applicable university policies.
It is the responsibility of the student to be cognizant and abide by the rules, regulations, and policies described in this handbook. Any questions or concerns should be directed to the program director. When the handbook does not cover a specific circumstance or the interpretation is not clear, the program director will make necessary decisions or interpretations.
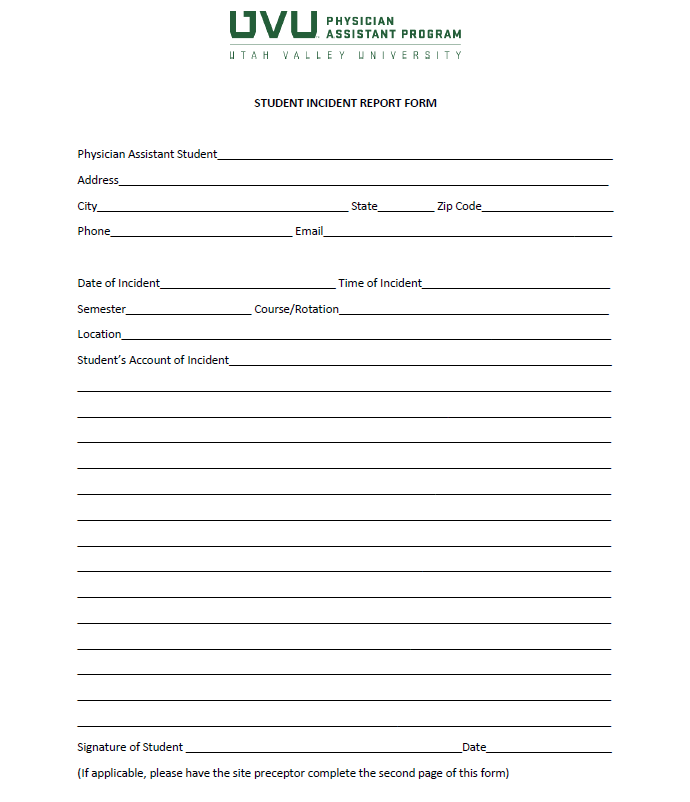
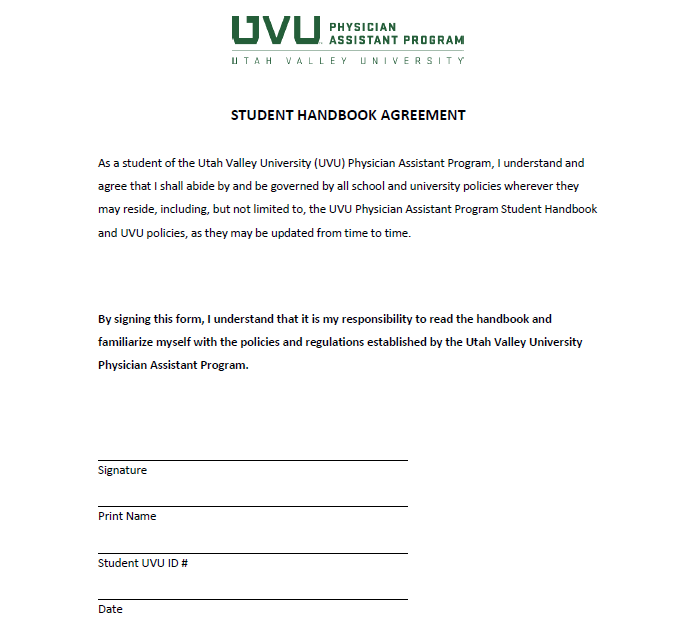
Students are expected to remain current on all policies and procedures of the university and those specific to the program throughout their enrollment in the program. This handbook will be reviewed during orientation. At orientation, the student will sign an acknowledgement form which states that the student agrees to follow program and university policies and procedures throughout their enrollment. Students will be given ample time to review this handbook prior to signing the acknowledgement form (see Appendix M).

2
UVU MISSION AND VALUES
Utah Valley University is an integrated university and community college that educates every student for success in work and life through excellence in engaged teaching, services, and scholarship.
UVU's culture supports our mission of student success. Student success encompasses both terminal degrees and the holistic education of students, and we believe that we can fulfill this mission best in an environment that allows all individuals to thrive personally and professionally. To this end, UVU operates in accordance with three core values: exceptional care, exceptional accountability, and exceptional results.
UVU ESSENTIAL STUDENT LEARNING OUTCOMES
The Essential Learning Outcomes (ELOs) are a comprehensive set of learning goals that are fostered and developed across a student's entire educational experience. They reflect the knowledge, skills, and competencies needed to meet the challenges of an ever-changing and complex world. The ELOs prepare students for future employment, life, and citizenship. With the achievement of these outcomes, UVU graduates will possess breadth and depth of knowledge, highly developed intellectual and practical skills, commitment to personal and social responsibility, awareness of the interdependence of communities, and the ability to synthesize and apply their learning to solve complex real-world problems.

3
PROGRAM MISSION
The mission of the Physician Assistant Program at Utah Valley University is to graduate academically and clinically prepared compassionate providers who strengthen our regional healthcare workforce through exceptional patient care.

4
PROGRAM GOALS
A3.12b, A3.12c

5
ACCREDITATION
The ARC-PA has granted Accreditation-Provisional status to the Utah Valley University Physician Assistant Program sponsored by Utah Valley University.
Accreditation-Provisional is an accreditation status granted when the plans and resource allocation, if fully implemented as planned, of a proposed program that has not yet enrolled students, appear to demonstrate the program’s ability to meet the ARC-PA Standards or when a program holding Accreditation-Provisional status appears to demonstrate continued progress in complying with the Standards as it prepares for the graduation of the first class (cohort) of students.
Accreditation-Provisional does not ensure any subsequent accreditation status. It is limited to no more than five years from matriculation of the first class.
The program’s accreditation history can be viewed on the ARC-PA website at http://www.arc-pa.org/accreditation-history-ut-valley-u/
Utah Valley University is accredited by the Northwest Commission on Colleges and Universities.

6
UVU PA PROGRAM DESCRIPTION
The PA program at UVU is a full-time, 28-month, year-round graduate program, consisting of 95 credit hours completed over seven semesters. The curriculum structure is specially designed to prepare students with the knowledge, skills, and confidence to become competent PAs who demonstrate interpersonal and communication skills that result in more effective and compassionate patient care.
All PA didactic courses are offered and must be fulfilled on location at UVU west campus. There are no provisions for substituting or waiving program courses.
UVU confers a Master of Physician Assistant Studies degree to students upon successful completion of all program requirements which include:
Students are required to participate in all program activities, comply with all program and university policies, and demonstrate professional behavior as defined in this student handbook. Students are assessed through a variety of methods that include written examinations, objective structured clinical examinations (OSCEs), practical workshops, written and oral assignments, and group presentations. Students must pass each component of the curriculum to make satisfactory progress in the program.
| SPRING 1 | COURSE TITLE | CREDIT HOURS |
| PAS 6701 |
Human Anatomy for the Physician Assistant I Course Description: Provides an in-depth, graduate-level understanding of human anatomy using a regional approach with instruction via lecture, simulation, and prosected cadavers. Helps students correlate the interactions between diverse structures and systems. Aligns content with the clinical medicine series. This is the first in a three-course series. Learning Outcomes:
|
1 |
| PAS 6711 |
Physiology / Pathophysiology for the Physician Assistant I Course Description: Examines how the human body functions from the cellular level to the interaction of organs and systems. Introduces functions related to anatomy and associations with common dysfunctions and diseases. Delivers course content in an organ system-based approach with the goal of preparing physician assistant students for clinical practice. Aligns content with the clinical medicine series. This is the first in a three-course series. Learning Outcomes:
|
2 |
| PAS 6721 |
Clinical Medicine I Course Description: Provides an in-depth, graduate-level understanding of human anatomy using a regional approach with instruction via lecture, simulation, and prosected cadavers. Helps students correlate the interactions between diverse structures and systems. Aligns content with the clinical medicine series. This is the second in a three-course series. Learning Outcomes:
|
3 |
| PAS 6731 |
Pharmacology / Pharmacotherapy for the Physician Assistant I Course Description: Applies clinical principles of pharmacology, pharmacokinetics, and pharmacodynamics. Focuses on the concepts of pharmacotherapy necessary for clinical prescribing decisions and includes discussion about side effects, complications, dosages, and contraindications. Aligns content with the clinical medicine series. This is the first in a four-course series. Learning Outcomes:
|
3 |
| PAS 6741 |
Clinical Skills I Course Description: Teaches the knowledge and skill set needed for history taking, focused and comprehensive physical examination, and use of diagnostic studies. Emphasizes patient dignity and autonomy as well as provider communication skills. Develops oral and written documentation skills appropriate for medical records. Aligns content with the clinical medicine series. This is the first in a three-course series. Learning Outcomes:
|
4 |
| PAS 6771 |
Physician Assistant Profession Course Description: Introduces the origin of the PA profession, PA professional organizations, and the culture of American medicine. Covers topics including credentialing, certification, team-based care, and the future trends of the PA profession. Learning Outcomes:
|
2 |
| PAS 6751 |
Clinical Decision Making I Course Description: Provides students the opportunity to work through clinical scenarios coinciding with the clinical medicine series and content covered in other courses within a small group, case-based setting. This is the first in a three-course series. Learning Outcomes:
|
1 |
| Total | 16 |
| SUMMER 1 | COURSE TITLE | CREDIT HOURS |
| PAS 6702 |
Human Anatomy for the Physician Assistant II Course Description: Provides an in-depth, graduate-level understanding of human anatomy using a regional approach with instruction via lecture, simulation, and prosected cadavers. Helps students correlate the interactions between diverse structures and systems. Aligns content with the clinical medicine series. This is the second in a three-course series. Learning Outcomes:
|
1 |
| PAS 6712 |
Physiology / Pathophysiology for the Physician Assistant II Course Description: Examines how the human body functions from the cellular level to the interaction of organs and systems. Introduces functions related to anatomy and associations with common dysfunctions and diseases. Delivers course content in an organ system-based approach with the goal of preparing physician assistant students for clinical practice. Aligns content with the clinical medicine series. This is the second in a three-course series. Learning Outcomes:
|
2 |
| PAS 6722 |
Clinical Medicine II Course Description: Teaches students to recognize, diagnose, and manage common medical conditions covering all organs and systems. Organizes the clinical medicine course series content into sets of modules. This is the second in a four-course series. Learning Outcomes:
|
3 |
| PAS 6732 |
Pharmacology / Pharmacotherapy for the Physician Assistant II Course Description: Applies clinical principles of pharmacology, pharmacokinetics, and pharmacodynamics. Focuses on the concepts of pharmacotherapy necessary for clinical prescribing decisions and includes discussion about side effects, complications, dosages, and contraindications. Aligns content with the clinical medicine series. This is the second in a four-course series. Learning Outcomes:
|
3 |
| PAS 6742 |
Clinical Skills II Course Description: Teaches the knowledge and skill set needed for history taking, focused and comprehensive physical examination, and use of diagnostic studies. Emphasizes patient dignity and autonomy as well as provider communication skills. Develops oral and written documentation skills appropriate for medical records. Aligns content with the clinical medicine series. This is the second in a three-course series. Learning Outcomes:
|
3 |
| PAS 6761 |
Behavioral Medicine Course Description: Focuses on how to identify, diagnose, and manage patients with a variety of mental and behavioral disorders in diverse populations across the lifespan. Covers topics such as normal and abnormal development, domestic violence, end of life care, diversity in medicine, health literacy, mental and behavioral disorders, as well as substance abuse. Learning Outcomes:
|
3 |
| PAS 6752 |
Clinical Decision Making II Course Description: Provides students the opportunity to work through clinical scenarios coinciding with the clinical medicine series and content covered in other courses within a small group, case-based setting. This is the second in a three-course series. Learning Outcomes:
|
1 |
| Total | 16 |
| FALL 1 | COURSE TITLE | CREDIT HOURS |
| PAS 6703 |
Human Anatomy for the Physician Assistant III Course Description: Provides an in-depth, graduate-level understanding of human anatomy using a regional approach with instruction via lecture, simulation, and prosected cadavers. Helps students correlate the interactions between diverse structures and systems. Aligns content with the clinical medicine series. This is the third in a three-course series. Learning Outcomes:
|
1 |
| PAS 6713 |
Physiology / Pathophysiology for the Physician Assistant III Course Description: Examines how the human body functions from the cellular level to the interaction of organs and systems. Introduces functions related to anatomy and associations with common dysfunctions and diseases. Delivers course content in an organ system-based approach with the goal of preparing physician assistant students for clinical practice. Aligns content with the clinical medicine series. This is the third and final course in this series. Learning Outcomes:
|
2 |
| PAS 6723 |
Clinical Medicine III Course Description: Teaches students to recognize, diagnose, and manage common medical conditions covering all organs and systems. Organizes the clinical medicine course series content into sets of modules. This is the third in a four-course series. Learning Outcomes:
|
3 |
| PAS 6733 |
Pharmacology / Pharmacotherapy for the Physician Assistant III Course Description: Applies clinical principles of pharmacology, pharmacokinetics, and pharmacodynamics. Focuses on the concepts of pharmacotherapy necessary for clinical prescribing decisions and includes discussion about side effects, complications, dosages, and contraindications. Aligns content with the clinical medicine series. This is the third in a four-course series. Learning Outcomes:
|
3 |
| PAS 6743 |
Clinical Skills III Course Description: Teaches the knowledge and skill set needed for history taking, focused and comprehensive physical examination, and use of diagnostic studies. Emphasizes patient dignity and autonomy as well as provider communication skills. Develops oral and written documentation skills appropriate for medical records. Aligns content with the clinical medicine series. This is the third and final course in this series. Learning Outcomes:
|
3 |
| PAS 6762 |
Personal and Clinical Leadership Course Description: Introduces the foundations of professional practice and leadership in the clinical setting. Includes the principles of managing conflict, self-reflection, mindful practice, and patient safety awareness in clinical practice. Learning Outcomes:
|
3 |
| PAS 6753 |
Clinical Decision Making III Course Description: Provides students the opportunity to work through clinical scenarios coinciding with the clinical medicine series and content covered in other courses within a small group, case-based setting. This is the third and final course in this series. Learning Outcomes:
|
1 |
| Total | 16 |
| SPRING 2 | COURSE TITLE | CREDIT HOURS |
| PAS 6724 |
Clinical Medicine IV Course Description: Teaches students to recognize, diagnose, and manage common medical conditions covering all organs and systems. Organizes the clinical medicine course series content into sets of modules. This is the fourth and final course in this series. Learning Outcomes:
|
1 |
| PAS 6734 |
Pharmacology / Pharmacotherapy for the Physician Assistant IV Course Description: Applies clinical principles of pharmacology, pharmacokinetics, and pharmacodynamics. Focuses on the concepts of pharmacotherapy necessary for clinical prescribing decisions and includes discussion about side effects, complications, dosages, and contraindications. Aligns content with the clinical medicine series. This is the fourth and final course in this series. Learning Outcomes:
|
3 |
| PAS 6772 |
Special Populations Course Description: Teaches the knowledge and skill set needed for history taking, focused and comprehensive physical examination, and use of diagnostic studies and assessment tools for patient populations with unique characteristics. Emphasizes shared decision-making, cultural awareness, and vulnerabilities of patient populations covered in this course. Learning Outcomes:
|
3 |
| PAS 6773 |
Health Promotion and Disease Prevention Course Description: Teaches the basic principles of wellness, health promotion, and disease prevention in the clinical setting. Covers topics including epidemiology, screening for common preventable diseases, interventions (in some cases), as well as complementary and alternative medicine. Learning Outcomes:
|
3 |
| PAS 6774 |
Supplemental Topics in Medicine Course Description: Examines specialized topics in patient care with emphasis on collaboration with other healthcare professionals. Includes topics in nutrition, genetics, dental health, and team-based care. Learning Outcomes:
|
1 |
| PAS 6775 |
Health Care Delivery Systems and Medical Ethics Course Description: Provides an overview of the United States healthcare delivery system, healthcare policy, quality care, patient safety, and prevention of medical errors. Reviews the role of the physician assistant in the healthcare system. Learning Outcomes:
|
2 |
| PAS 6781 |
Capstone I Course Description: Mentors students in creating the foundation for a robust professional portfolio based on competency domains and entrustable professional activities. Helps students develop the ability to critically review medical literature and determine what skills and training are most needed for a selected area of interest. This is the first in a three-course series. Learning Outcomes:
|
1 |
| PAS 6790 |
Family Medicine I – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in practicing the principles of family medicine. Facilitates experience in outpatient evaluation of patients across the lifespan (infant, child, adolescent, adult, and elderly) including preventive medicine and acute and chronic illness. This course is a five-week supervised clinical practical experience (SCPE) and the course syllabus reflects both the first and second courses in this series. May be graded credit/no credit. Learning Outcomes:
|
3 |
| Total | 17 |
| SUMMER 2 | COURSE TITLE | CREDIT HOURS |
| PAS 6792 |
Behavioral and Mental Health Care – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with an opportunity to learn, understand, and gain clinical experience in practicing the principles of behavioral and mental health care conditions. Facilitates experience in outpatient / inpatient evaluation of patients across the lifespan (adolescent, adult, and elderly) including acute and chronic illness. This course is a five-week supervised clinical practical experience (SCPE). May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6793 |
Women's Health – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in managing common gynecologic disorders. Includes obstetrical experience with routine prenatal and postpartum care, and may include labor and delivery. Comprises women’s health care in an inpatient / outpatient setting across the lifespan (adolescent, adult, and elderly) including preventive medicine and acute and chronic illness. This course is a five-week supervised clinical practical experience (SCPE). May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6794 |
Pediatrics – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in practicing the principles of pediatric medicine. Facilitates experience in outpatient evaluation of patients across the lifespan (prenatal, neonatal, infant, child, adolescent) including preventive medicine and acute and chronic illness. This course is a five-week supervised clinical practical experience (SCPE). May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6782 |
Capstone II Course Description: Mentors students in initiating a robust professional portfolio. Helps students create a single space where all documentation of competency will be organized and accessible. Prepares students to work independently and in teams to further skills and training relevant to selected areas of interest. This is the second in a three-course series. Learning Outcomes:
|
1 |
| Total | 10 |
| FALL 2 | COURSE TITLE | CREDIT HOURS |
| PAS 6795 |
Emergency Medicine – Supervised Clinical Practice Experience Course Description: PProvides the physician assistant student with clinical experience in practicing the principles of emergency medicine. Facilitates experience in the evaluation of patients across the lifespan (infant, child, adolescent, adult, and elderly). Includes learning skills needed for appropriate triage, stabilization, diagnosis, and management of patients with significant traumatic injuries, acute illnesses, acute complications of chronic illnesses, as well as the management of less life-threatening problems. This course is a five-week supervised clinical practical experience (SCPE). May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6796 |
Surgery – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in practicing the principles of surgery. Facilitates experience in pre-operative, intra-operative, and post-operative evaluation and management of patients across the lifespan (adolescent, adult, and elderly) including acute, chronic, and emergent conditions in the inpatient, outpatient, and operating room settings. This course is a five-week supervised clinical practical experience (SCPE). May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6797 |
Internal Medicine – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in practicing the principles of internal medicine. Facilitates experience in either an outpatient setting, inpatient setting, or a combination of both, caring for adult and elderly patients with acute, chronic, and/or preventive care needs. This course is a five-week supervised clinical practical experience (SCPE). May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6783 |
Capstone III Course Description: Mentors students in completing a robust professional portfolio. Helps students finalize a single space where all documentation of competency will be organized and accessible for potential employers and future growth. Prepares students to work independently and in teams to show skills and training relevant to selected areas of interest. This is the third and final course in this series. Learning Outcomes:
|
1 |
| Total | 10 |
| SPRING 3 | COURSE TITLE | CREDIT HOURS |
| PAS 6791 |
Family Medicine II – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in practicing the principles of family medicine. Facilitates experience in outpatient evaluation of patients across the lifespan (infant, child, adolescent, adult, and elderly) including preventive medicine and acute and chronic illness. This course is a five-week supervised clinical practical experience (SCPE) and the course syllabus reflects both the first and second courses in this series. May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6798 |
Elective Rotation I – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in a specific area of interest approved by the faculty from a variety of surgical, family medicine, or internal medicine specialties or subspecialties. Enables students to learn to recognize conditions treated by these specialties, so they can refer patients appropriately and/or work in a supportive role for such specialists. This course is a five-week supervised clinical practical experience (SCPE). May be repeated for a maximum of 6 credits toward graduation. May be graded Credit / No Credit. Learning Outcomes:
|
3 |
| PAS 6799 |
Elective Rotation II – Supervised Clinical Practice Experience Course Description: Provides the physician assistant student with clinical experience in a specific area of interest approved by the faculty from a variety of surgical, family medicine, or internal medicine specialties or subspecialties. Enables students to learn to recognize conditions treated by these specialties, so they can refer patients appropriately and/or work in a supportive role for such specialists. This course is a five-week supervised clinical practical experience (SCPE). May be repeated for a maximum of 6 credits toward graduation. May be graded credit/no credit. Learning Outcomes:
|
3 |
| PAS 6776 |
Physician Assistant Practice Course Description: Prepares the physician assistant to enter clinical practice. Covers applications for PANCE and National Provider Identification (NPI) numbers. Focuses on the importance of accurate and complete documentation related to patient care. Teaches students to create customized career development tools. Includes a PANCE review course. Learning Outcomes:
|
1 |
| Total | 10 | |
| Total Program Hours | 95 |
YEAR 1: SEMESTERS 1 – 3
The first year of the program consists of three didactic semesters designed to prepare students for clinical experience by developing their physical examination techniques and diagnostic skills and learning about common medical conditions in a system-based format. Students will also receive instruction in health issues specific to the local community, patient education, and the PA profession.
YEAR 2: SEMESTER 4
The 4th semester is a combination of didactic curriculum and the first Supervised Clinical Practice Experience (SCPE). The first 12 weeks are in the classroom focusing on advanced medicine topics in special populations (geriatrics, pediatrics, emergency room) and the management of conditions associated with those populations and preparation for practice focusing on care in the surgical setting. The first SCPE will occur during the last four weeks of the 4th semester.
YEAR 2 AND 3: SEMESTERS 5 – 7
The final three semesters of the program will continue with SCPEs #2-10 with post clinical activities and didactic course work presented online and during the break between each rotation. Clinical training sites and preceptors are established and monitored by the program. Students will work a minimum of 40 hours per week at their site. A mandatory orientation will be held prior to students starting their clinical year. At the conclusion of every core rotation, students will take a mandatory End of Rotation written examination. Students will also participate in four mandatory Return Visits (RV) involving lectures, workshops, and engaged learning experiences that will develop students as professionals and provide supplemental learning.
PAPERLESS PROGRAM
Program operations, teaching materials, and assessments will be executed in electronic form whenever possible, including:
Students are responsible for any costs if they choose to buy books or other materials outside of what is provided by the program. Students must obey all copyright laws.
IPAD with APPLE PENCIL or LAPTOP or PC with a TOUCHSCREEN
Students are required to have an iPad with Apple Pencil or a laptop or PC with a touchscreen upon enrollment. Recommended applications include:
As a courtesy to the instructor, peers, and guests, students should not use their electronic resources for personal activities (such as shopping, checking email or social media) during lectures or other educational activities.
SUBSTITUTION/WAIVER OF COURSEWORK
A3.16a,b,c
Advanced placement is defined as a waiver of required professional coursework in the PA program, and will not be granted under any circumstances. All students who enter the program must fulfill all program requirements. All courses within the curriculum are required. No transfer credit is accepted. No credit is granted for pre-admission experiential learning, prior coursework, degrees, certifications, or advanced training.

7
UVU PA PROGRAM CONTACT INFORMATION
The following is a listing of the program’s principal faculty and staff with their contact information. To reach other members of the program (including part-time instructors or other staff), students may call the program office at 801-863-7982.
ARC-PA accreditation refers to full-time faculty as “principal faculty.” In addition to principal faculty, the program utilizes instructional faculty from other departments in UVU as well as community professionals with expertise in healthcare and other valuable experience.
| Principal Faculty | Phone | |
| Program Director Karen Mulitalo, MPAS, PA-C Assistant Professor |
[email protected] | 801-863-7563 |
| Director of Didactic Education Jim Sutton, MPAS, PA-C Assistant Professor |
[email protected] | 801-863-4671 |
| Director of Clinical Education Shaun Young, MPAS, PA-C Assistant Professor |
[email protected] | 801-863-7966 |
| Director of Student Affairs Summer Karafiath, MD Assistant Professor |
[email protected] | 801-863-7259 |
| Faculty Cydne Evan, MPAS, PA-C Assistant Professor |
[email protected] | 801-863-7623 |
| Faculty Jonathan Nelson, MPAS, PA-C Assistant Professor |
[email protected] | 801-863-8595 |
| Faculty Ryan Baker, MPAS, PA-C Assistant Professor |
[email protected] | 801-863-6877 |
| Staff | Phone | |
| Director of Admissions Keri Hensley |
[email protected] | 801-863-7063 |
| Administrative Assistant Evie Mecham |
[email protected] | 801-863-8586 |
| PA SIM Technician Sharla Washburn |
[email protected] | 801-863-7982 |
| Clinical Education Coordinator Emily Mecham |
[email protected] | 801-863-7990 |
| Clinical Specialist Natalie Ellis, MPAS, PA-C |
[email protected] | 801-863-7982 |
| Medical Director | Phone | |
| Medical Director Gary Sanderson, DO |
[email protected] | 801-863-7982 |

8
FACULTY ADVISORS
The program’s principal faculty and staff are committed to providing support and assistance to every student. The following UVU PA Program policies have been formulated to ensure the continuance of this commitment.
Each student is assigned a faculty advisor for the duration of his/her tenure in the program. Students will meet with their advisor at least once a semester for academic and professional advisement. This ensures that all students have continuity and equal access to an advisor. Faculty advisors serve as valuable resources for answering professional questions and providing counseling and advisement.
The role of the faculty advisor is to:
Faculty advisors are also able to provide students with appropriate referrals and resources within the wider UVU community (e.g., psychological counseling and financial aid). Should students need referral to counseling or services for personal needs on or off campus, these referrals can be made by the faculty advisor, Student Progress Committee (SPC) or by the student as a self-referral.
Should students feel they need advisement on a referral for personal needs, faculty advisors are available during weekly scheduled office hours, by appointment, or upon request. It is imperative that students keep their advisor apprised of any situation that may jeopardize their successful academic or professional progression in the program, so the faculty advisor can help render assistance as soon as possible. The faculty advisors are committed to your success in the program and will help you find the resources you need to be successful.
Principal faculty, program director, and medical directors are prohibited from participating as medical providers for participants in the program, except in case of an emergency.

9
TECHNICAL STANDARDS
A3.13e
The goal of the program is to prepare students to become competent, caring physician assistants possessing the skills for lifelong learning necessary to incorporate new knowledge and methods into medical practices required to adapt to the changing professional environment. All students admitted to the program are expected to continually demonstrate the specific technical standards specified below. These technical standards are considered to be prerequisites for admission, for progression throughout the program, and to qualify for graduation from the UVU PA Program.
Every physician assistant student must be able to perform independently, with or without reasonable accommodation, a diversity of skills related to effective performance as a professional student and health care practitioner in training. A detailed description of those essential functions and technical standards required of each physician assistant student are described below:
Admitted students who have a disability and need accommodation should initiate discussions with the Office of Accessibility Services as soon as the offer of admission is received and accepted. Each student must be fully cognizant of the technical standards. Questions or concerns about the technical standards should be discussed with the program director. If a health condition arises that would in any way alter the student’s ability to perform in the didactic or clinical setting, it is the student’s responsibility to report this immediately to the program director. See the UVU PA Program Technical Standards Student Attestation Form in (Appendix A).

10
HEALTH CLEARANCES AND INSURANCE
A3.07a
To ensure the safety of students, faculty, staff, clinical personnel, and patients and to comply with clinical affiliation agreement mandates, no student will be permitted to matriculate into the program or participate in clinical rotations unless they have received health clearance by a qualified medical provider. The health clearance is described below and is based on current Centers for Disease Control and Prevention (CDC) recommendation for health professionals, and reflects Utah State specific mandates which mirror the CDC recommendations.
Additionally, all students must provide evidence of health insurance coverage for matriculation and participation in the clinical year. It is the student’s responsibility to ensure that the health clearance and insurance is obtained, and it is the program’s responsibility to verify the information.
HISTORY AND PHYSICAL EXAMINATION
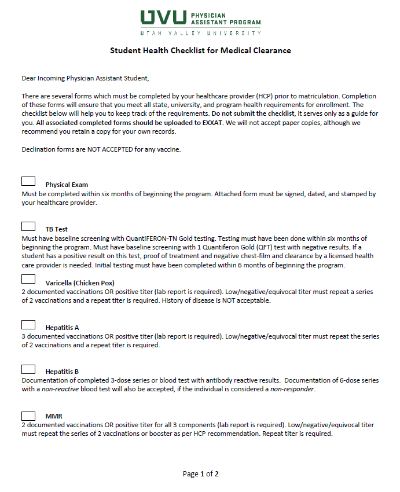
To be medically cleared prior to matriculation, students must complete all requirements on the Student Health Checklist see (Appendix B) that is available on Exxat. Documentation will be uploaded into Exxat and kept encrypted and secure.
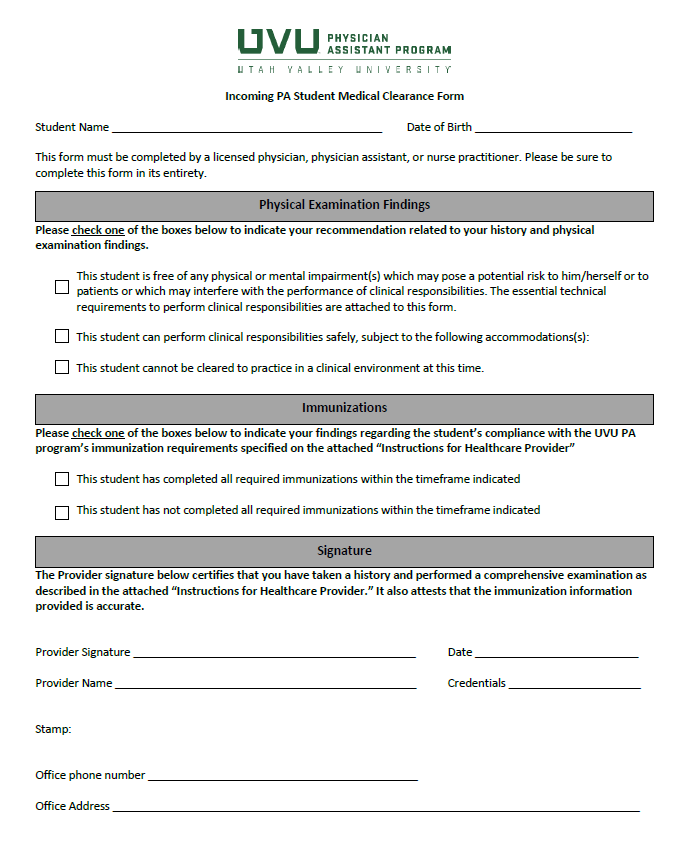
As part of the health clearance, students are required to undergo a comprehensive physical examination to ensure that they are equipped to meet the demands of a career in healthcare. It is not necessary to provide a full report of this examination. Students will provide the medical provider with the instructions letter see (Appendix C) and have the provider indicate their recommendation on the Medical Clearance Form see (Appendix D). This needs to be completed prior to matriculation.
THE ASSESSMENT SHOULD INCLUDE:
HEALTH INSURANCE
All PA students are required to carry health insurance coverage. A copy of verification of insurance must be submitted to the program prior to matriculation and prior to the start and end of the clinical year.
Failure to complete any of these required items by the due date may result in revoking the seat invitation to the program, a delayed start to the clinical year, and/or delayed clinical site placements. This may in turn delay the student’s completion of the program and may result in additional tuition and or fees. See the "Registration and Tuition" section of this handbook.
Some clinical rotations have additional requirements which students will also be required to complete prior to starting the specific rotation (i.e. interview, orientation, and time specific background checks/drug testing or physical exam). Students may incur additional costs in order to complete rotation specific clearance requirements. The Clinical Team will inform the student of rotation assignments through EXXAT two to three months in advance and will discuss any additional requirements at that time.

11
REQUIRED IMMUNIZATIONS AND TESTS
A3.07a,b
Immunization and TB testing compliance is required of all PA students. These vaccinations are based on current Center for Disease Control (CDC) recommendations and Utah state guidelines. Utah State guidelines follow the CDC’s recommendations. For current CDC’s recommended vaccinations for health care providers, please see https://www.cdc.gov/vaccines/adults/rec-vac/hcw.html
PA students are at risk for exposure to, and possible transmission of, diseases due to their contact with patients or with infective material of patients. Student compliance with immunizations and testing is required to matriculate and remain in the program.
PA students are required to submit copies of official proof of the required immunizations/tests to the program. If unable to find childhood immunization records, students may get a blood test (titer). We suggest beginning the immunization verification process early in order to meet the Program deadlines. Declination forms are NOT ACCEPTED for any vaccine.
Students without completed forms will not be permitted to participate in courses, assignments, or clinical rotations. Failure to complete and provide evidence of completion of the onboarding requirements may delay the student’s progress in the program. Immunization requirements are subject to change based on agency and/or infection control requirements where students are assigned to do clinical rotations. To participate in the clinical component of the physician assistant program, students will be required to abide by the immunization, health screening, and drug testing requirements of our clinical program partner sites, subject to individual accommodations. If placement at alternative clinical sites is not an available accommodation, the only available accommodations from UVU may be deferral or temporary withdrawal from the program.
UVU PA Program currently has no international travel requirements for students or elective international curricular components.
PROOF OF IMMUNIZATION/TEST REQUIREMENTS:
| Test Name | Parameters |
| Tdap | Must be within 10 years. Must include pertussis, Td not accepted. |
| Measles/Mumps/Rubella (MMR) |
2 documented vaccinations OR positive titer for all 3 components (lab report is required). Low/negative/equivocal titer must repeat the series of 2 vaccinations or booster as per HCP recommendation. Repeat titer is required. |
| Hepatitis A |
2 documented vaccinations OR positive titer (lab report is required). Low/negative/equivocal titer must repeat the series of 2 vaccinations and a repeat titer is required. |
| Hepatitis B | Documentation of completed 3-dose series and blood test with antibody reactive results. Low/negative/equivocal titer must repeat the series of 2 Heplisav B OR 3 Energix vaccinations. |
| Varicella (Chicken Pox) | 2 documented vaccinations OR positive titer (lab report is required). Low/negative/equivocal titer must repeat a series of 2 vaccinations, and a repeat titer is required. History of disease is NOT acceptable. |
| Influenza | One dose annually at the beginning of the flu season around September or October. The flu season begins in October and extends through the winter/spring semester. If a student is unable to receive the vaccination, the student must wear a protective mask for each patient encounter during the entire flu season. |
| TB Test | Must have baseline screening with a Quantiferon Gold (QFT) test or purified protein derivative (PPD) skin test with negative results. If a student has a positive result on this test, proof of treatment and negative chest-film and clearance by a licensed health care provider is needed. Initial testing must have been completed within 6 months of beginning the program. |
| Polio | 3 documented vaccinations (primary series) OR a positive titer (lab report is required). Childhood immunizations are accepted. If negative titer, the student should contact the program. |
| Covid-19 Vaccines | Recommendation of at least 1 completed FDA approved Covid-19 vaccination prior to matriculation. |

12
DRUG SCREENING
Health care providers are entrusted with the health, safety, and welfare of patients, have access to controlled substances and confidential information, and operate in settings that require the exercise of good judgment and ethical behavior. For this reason, clinical facilities that serve as educational and training sites for students increasingly require drug screening for individuals who provide services within the facility and particularly for those individuals who provide patient care. In addition, many licensing agencies require that individuals pass a drug screen as a condition of licensure and/or employment. Thus, it is in the interest of both students and the program to identify and resolve potential issues where a student may not be allowed to participate in a clinical rotation due to the use of controlled or illegal substances.
For the above reasons, and because UVU’s PA program is a safety-sensitive program where others’ well-being depends, in part, on our students’ sound and attentive judgment, all students will be required to undergo a drug screen prior to enrollment in the program and again in preparation for clinical rotations. A negative drug screen, according to Utah laws regarding illegal substances, is required for matriculation in the program and participation in any clinical experience. Additionally, at any point in the program, a student may be requested to undergo an immediate, random drug screen. The program may re-screen students at any time.
Students enrolled in the program will receive information about the requirement for drug screening, deadlines for compliance, results reporting, and associated fees prior to matriculation and again prior to the start of the clinical year. In accordance with UVU policy 548, applicants to clinical programs at UVU must pass a drug test. Students will be tested upon acceptance to a clinical program. The responsibility for passing the drug test resides with the student regardless of possession of a medical cannabis card that is legal in any state. Clinical programs reserve the right to repeat drug tests at any time during the clinical program. The screening is managed by Exxat/Universal Background Screening. Students will receive communication from Exxat/Universal with instructions and deadlines for the screening.
Results of the student drug screen will be reported to the program director. Students who receive a positive screen will be reviewed by the program director and/or university’s General Counsel and students who test positive are subject to UVU policies. See (UVU Alcohol/Drug Campus Policy). Any student found to be in violation of the drug policy may be dismissed from the program. Students who refuse to submit to any required drug screen will be dismissed from the program.
To participate in the clinical component of the physician assistant program, students will be required to abide by the immunization, health screening, and drug testing requirements of our clinical program partner sites, subject to individual accommodations. If placement at alternative clinical sites is not an available accommodation, the only available accommodations from UVU may be deferral or temporary withdrawal from the program.
A violation is defined as:

13
BACKGROUND CHECK
On January 1, 2004, the Joint Commission on Accreditation of Healthcare organizations (JCAHO) instituted new regulations that must be followed for hospitals, home health agencies, clinics, etc., to gain or maintain accreditation status. One of these regulations requires that all individuals who are involved with inpatient care activities, i.e., employees, volunteers and students, must have criminal background checks as well as other healthcare-related checks (e.g., up-to-date vaccinations, TB tests).
All students will be required to undergo a criminal background check prior to matriculation, prior to the start of the clinical year, and at the end of the clinical year. Matriculation into and continuation within the program is dependent on an acceptable background check and is at the discretion of the program director.
Further, any infractions may prevent continuation in the didactic phase of the program, delay or prevent clinical placement and/or graduation. Should an incident occur at any time during the program, the student must self-report the incident to the program director immediately. Students who refuse to submit to the required background checks will be dismissed from the program.
Students enrolled in the program will receive information about the requirements for background check, deadlines for compliance, results reporting, and associated fees prior to matriculation and again prior to the start of the clinical year. The screening is managed by Exxat/Universal Background Screening.

14
REGISTRATION AND TUITION
Registration and Payments
Registration for classes is completed online through the students' myUVU page. Registration notifications are sent electronically to student’s UVU email account. Registration instructions are available online at https://www.uvu.edu/registration/
All tuition and fees are payable to the university’s cashier/bursar's office at the time of registration. Payment instructions are available online at https://www.uvu.edu/cashier/
Checks for more than the total tuition and fees due will not be accepted. Payment should be submitted by the specified per session due dates. Late fees may be applied to late registration and/or late payments. If payment is not received by the due date, students are automatically removed from course rosters. Outstanding balances with UVU may result in collection actions and will result in a hold on the student’s account preventing future registration and ordering UVU official transcripts. Students with outstanding payments may be barred from class, examinations, or clinical assignments and/or suspended from all program activities until payments are made.
It is the responsibility of the student to notify the program if he/she has difficulty maintaining registration. Students dismissed from the university for failure to maintain registration may not be allowed to return to the program at a later date.
TUITION
Tuition and student fees are established by the Utah State Board of Regents. Tuition, fees, and additional expenses as they appear in the catalog are subject to change and are based on the current school year rates. Any changes to these expenses will be determined after the annual program review process is concluded. Handbook/website revisions will coincide with the opening of CASPA. Candidates will have the opportunity to review the most up to date version. However, revisions may be made on an emergency basis with extenuating circumstances (e.g. change in state law or university policy).
The table below details anticipated tuition, fees, program required expenses, as well as other costs associated with the program for the entering Spring cohort. Additional fees may be associated with financial aid. All costs are estimated.
| Tuition | |
|---|---|
| Utah Resident Program Tuition | $85,000 |
| Non-Utah Resident Program Tuition | $131,000 |
| *Non-Utah Resident students pay Utah Resident tuition during Summer Semesters Student receives residency after 1 year |
*$106,000 |
| University Fees ($360 per semester) | $2,520 |
| Total Estimated Tuition & Fees Utah Residents | $87,520 |
| Total Estimated Tuition & Fees Non-Utah Residents | $133,520 |
| *If student receives Utah residency after 1 year | *$108,520 |
| Additional Program Estimated Costs and Fees/Student Responsibilities | |
|---|---|
| Non-refundable Graduate Matriculation Fee | $1,000 |
| Textbooks/Resources/Miscellaneous Supplies | $2,000 |
| Diagnostic Medical Equipment | $1,500 |
| Training and Certifications | $350 |
| Scrubs, white coat and professional dress | $250 |
| iPad/Pencil | $1,500 |
| Immunizations, Annual TB Test, Flu Shot | $250 |
| Medical Insurance (Required) | $2,700 |
| Professional Liability Coverage (University will provide) | $0 |
| Estimated Living and Transportation Expenses Per Semester | |
|---|---|
| Housing and Food | $4,509 |
| Miscellaneous Living Expenses | $729 |
| Student Conference Fees | $250 |
| Free UTA pass available | $0 |

15
TUITION REFUNDS
A1.02k
Refunds are not automatic. The tuition refund policy is established by the Utah State Board of Regents and amended by each college or university to fit their programs. The Utah Valley University (UVU) refund policy can be found on the UVU Tuition Policies & Procedures webpage.
UVU refunds to students who withdraw from school or drop classes are as follows:
Semester
Exact dates for semester, block, and weekend classes can be found on the UVU Schedule webpage under Student Dates and Deadlines.
Students must drop classes or completely withdraw by the published 100% Refund Deadline to have the charges removed from their account. Students who withdraw after that date will not receive a refund. If a student has not paid his or her charges for the semester, he or she will continue to owe the university for these charges and will be subject to collections procedures if left unpaid.
Changes in enrollment may affect Financial Aid eligibility and amounts received. Financial Aid awards may be pulled back when dropping courses, thus increasing the amount owed.
A Petition to the Refund Policy Form can be obtained from the Office of the Registrar or visit the UVU Registration webpage.

16
BLS/ACLS AND OTHER REQUIRED CERTIFICATIONS
The following certifications and training will be required for participation in the student-run clinic during the didactic phase and in clinical rotations during the clinical phase.
BASIC LIFE SUPPORT (BLS)
The program will provide BLS certification through the American Heart Association prior to the clinical year. Proof of current BLS certifications is required prior to matriculation. Current certifications earned prior to the start of the program will be accepted if they are through the American Heart Association – no other will be accepted. ACLS certification is not a substitute for BLS certification. All certifications must be current and kept current while enrolled.
ADVANCED CARDIOVASCULAR LIFE SUPPORT (ACLS)
The program will provide ACLS certification through the American Heart Association prior to the clinical year. Current certifications earned prior to the start of the program will be accepted if they are through the American Heart Association – no other will be accepted. All certifications must be current and kept current while enrolled.
OTHER REQUIRED CERTIFICATIONS AND TRAINING
These certifications may be required prior to matriculation and will be provided by the program prior to the clinical year:

17
STUDENT EMPLOYMENT
A3.04, A3.05ab, A3.15e
The UVU PA Program is a rigorous, full-time academic program. It is strongly recommended that students not accept or continue outside employment while enrolled in the program.
Students are not permitted to work for the program or perform any clerical or administrative duties for the program. Students are not permitted to substitute or function as instructional faculty.
Students with prior knowledge or skills may assist other students but may not replace the primary instructor with any component of the curriculum.
Students will not be required to perform any clerical or administrative work or teaching on behalf of the PA program during any clinical rotation. Students may not substitute for paid clinical staff while on rotation at any clinical site. The clinical director will continually monitor sites for adherence to this policy and notify the program director of any deviations to this policy.

18
PROGRAM COMMUNICATION
The structure of clinical education mandates an increased frequency of communication with students. The primary form of communication is via phone, Microsoft Teams, and the university email system. Communication will also occur via Canvas or other learning systems.
Official correspondence related to the program or the university to students is considered received by the student if sent to any one of the following:
MYUVU STUDENT EMAIL
Email is the primary and official means of communication from UVU to students. Once a student receives a myUVU student email account, official communication from the university is directed to that account.
Official communication contains information on conducting business with Utah Valley University and for which every student is held accountable. Students are expected to read communications in a timely fashion because communications often are time sensitive. Examples of official communication can include, but are not limited to:
All use of email must be consistent with local, state, and federal law, as well as other university policies and guidelines.
Student email accounts will remain active if the student is enrolled at UVU or is on an approved leave of absence.
COMMUNICATION GUIDELINES AND ETIQUETTE
To recognize and keep clear the roles of others in the academic or clinical team, students are encouraged to refer to all program faculty, staff, instructors, clinical preceptors, and administrators by their appropriate title (Dean, Dr, Mr., Ms., Professor, etc.)
COMMUNICATION WITH THE PROGRAM AND UNIVERSITY
Students, program staff, faculty, clinical preceptors, and other program personnel are expected to check messages daily, and return messages in a timely manner, generally within two (2) business days.
Faculty are available to meet with students by appointment during office hours or other non-class hours during the regular school week. Appointments should be arranged directly with the faculty member via phone or email.
EMAIL COMMUNICATION GUIDELINES
PHONE COMMUNICATION GUIDELINES
CONTACT INFORMATION
Students are required to provide the program with permanent contact information. Students are expected to notify the program immediately, as well as the Office of the Registrar, upon any change of contact data. Name changes should be submitted to the registrar with the Change of Personal Information form found on the UVU Registration webpage. It is not the responsibility of the program to confirm the accuracy of this information or report it to the registrar.
MYUVU STUDENT DASHBOARD
PA students have access to the online Student Center located at my.UVU.edu
My.UVU.edu is the university portal and provides single sign-on access to important systems. Many student services and tools are found on my.UVU.edu including class schedule, BookMatch, student deadlines, course catalog, and tuition, fees, & financial aid. UVU announcements and campus events can be found on the home page of my.UVU.edu.
STUDENT UVU ID
A UVU ID is a unique eight-digit number. Your UVU ID number is your username to login to UVU Login Services.
To find your UVU ID visit the UVU Campus Connection webpage.
CANVAS
Students use Canvas to access course syllabi, learn about and submit course assignments, access course materials, communicate with faculty, and review course grades. Canvas is available through my.UVU.edu.
For more information visit the UVU Office of Teaching and Learning webpage.
BANNER
Banner is the enterprise data system for the university. Students may access student services, financial aid, and personal information. Banner is accessed through the Student tab in my.UVU.edu.

19
PROFESSIONAL CONDUCT
UVU PA students are enrolled in a professional clinical training program and therefore must adhere to and demonstrate compliance with requirements and expectations of both the university and the program throughout their enrollment in the program.
Expectations of professionalism discussed in this handbook are assessed throughout student enrollment in the program. Students who fail to meet these expectations will be referred to the SPC. Certain lapses of professionalism and any disciplinary action may be revealed by the program when students apply for a license to practice as a PA, and can result in licensing delays, a restricted license, or denial of licensure. Any student whose actions directly or indirectly jeopardize the health and safety of patients, faculty, clinical site staff or fellow students will face disciplinary action including removal from the clinical site and/or program. Removal from a clinical rotation may prolong the length of the program and delay the student’s graduation.
As a part of maintaining satisfactory academic progress in the program, students must demonstrate professional behaviors. Standards of professional behavior are informed by the following:
PROFESSIONAL CONDUCT EXPECTATIONS
The following describes program expectations for professional behavior of PA students. For a PA student, professionalism is the skill, good judgment, and respectful and ethical behavior that is expected from a physician assistant who is trained to provide exceptional care. It is important that students conduct themselves in a highly professional manner consistent with patient-care responsibilities and interprofessional teamwork during their training in the program. Therefore, throughout all facets of their education and the program, PA students are required to develop and demonstrate the following:

20
DRESS CODE
How a student dresses expresses their respect for self and others, sensitivity to others, and commitment to health and safety. A student’s dress is a demonstration of their professionalism and an indication of the physician assistant they aspire to become. What constitutes appropriate attire varies depending on the setting. Classroom attire is generally more casual than what is expected in clinic, and special attire may be required for health and safety reasons in certain clinic and hospital settings.
CLASSROOM ATTIRE
Professional learners are entrusted with the responsibility for presenting themselves in a way that demonstrates incorporation of professionalism goals. These include awareness of legal or regulatory limits on dress, demonstration of respect and compassion for others, and consideration of sensitivity to age/culture/gender and ability of peers.
ANATOMY LAB ATTIRE
The following guidelines are attire that must be worn while in the anatomy lab while working with cadavers:
CLINIC ATTIRE
The following guidelines provide the minimum expectations of most patient-care settings. In addition to the classroom attire rules, all students must adhere to the following during clinical rotations:
Any clothing, hair color, jewelry, or body piercing that may cause concern with affiliated faculty, hospitals, or patients should be avoided. Preceptors and/or clinical sites may have site specific dress requirements, which students may be required to abide by.

21
MEDIA
SOCIAL MEDIA
All PA students must abide by the UVU Social Media Guidelines.
Many individuals participate in social media for a variety of reasons: to connect with professional networks, to find out what’s happening at other places, to enhance productivity and teambuilding, and to put together ad-hoc groups. Exchanging and sharing information can improve our personal and professional lives. However, social networking exposes one to an unsolicited audience and set of experiences. Continual attention is required to successfully manage personal and professional lives online.
The following are general policies regarding social networking as a PA student.
UVU PA PROGRAM USE OF STUDENT REPRESENTATION
Subject to UVU policies and the Family Educational Rights and Privacy Act, photos, audio, and video recordings of students may be taken for posting on the program web site or for publication to promote the activities of the program. To facilitate this process, students are encouraged to consent to being photographed, filmed or recorded by filling out the Creative Works License and Model Release Form, see (Appendix F). Students have the right to decline participation in the recording methods that may be viewed publicly and should speak directly with the program director as early as possible to accommodate this choice.
PHOTOGRAPHY, AUDIO AND VIDEO RECORDING
The program will use tools for student assessment and feedback in the form of digital audio-video recording, photography of lectures and student activities to enhance the learning experience and promote the program. However, recordings collected by the program of standardized patient encounters may be held for private viewing only. Students must never share or display, in whole or in part, recordings of standardized patient encounters.
Students must ask for permission before using cameras or electronic devices for recording program curricular activities. Portable electronic devices risk the transfer of these recordings to a non-secure, web-based media and may violate individual privacy and institutional intellectual property copyrights. Recorded material must not be posted on the Internet without appropriate authorization see (Social Media Guidelines above). These curricular activities include, but are not limited to: cadavers, simulation in Clinical Decision Making, Clinical Skills labs, Maliheh Free Clinic and other activities as designated by the program.
Current university policy is that all lectures will be recorded automatically and made available to be accessed by students. Students will not be allowed to record lectures on personal devices. Use of lectures recorded by the program are limited to personal or course study and may not be made public or shared. Video and photography are only permitted with permission of the person being recorded who has signed the Consent and Media Release Form.
Compliance with these policies is part of professionalism expectations that are assessed throughout the entirety of the program and are not limited to classroom activity. Failure to comply will be referred to SPC for evaluation and potential sanctions.
This policy does not affect non-curricular activities (breaks, independent study sessions off campus, etc.), however, even in these settings, students are expected to ask permission from individuals before photographing or recording.

22
UVU ALCOHOL, DRUGS AND TOBACCO POLICIES
UVU ALCOHOL/DRUG CAMPUS POLICY
Utah Valley University is a drug-free campus. Utah Valley University has developed an alcohol and tobacco and other drug policy not only in response to the federal drug-free legislation, but also to encourage and sustain an academic environment that promotes the health, safety, and welfare of all members of its community.
In keeping with these objectives, alcoholic beverages, unlawful drugs, and other illegal substances shall not be consumed, used, carried, sold, or unlawfully manufactured on any property or in any building owned, leased, or rented by UVU, or at any activity sponsored by the program (UVU Policies 155, 158, and 541).
Any faculty, staff member, or student who violates this prohibition, or who does not cooperate with the program in its attempts to maintain a drug-free environment, will face disciplinary action up to and including expulsion or dismissal from UVU and the UVU PA Program.
Individuals violating any town ordinances, state criminal laws, or federal laws relating to alcohol or drug use (including tobacco use) also are subject to substantial legal sanctions including fines and imprisonment.
If you are under the influence on UVU property, you will be subject to consequences, see UVU Student Rights & Accountability webpage.
For more information regarding the UVU’s alcohol, drug, and tobacco policies see UVU Alcohol/Drug Campus Policy webpage.
PA STUDENT IMPAIRMENT
Students represent the university and should always behave responsibly and professionally, on and off campus. Students must not appear at the university or clinical sites under the influence of any substance. A student who is convicted of any form of public intoxication, including driving while intoxicated, must immediately report that conviction to the program.

23
NONDISCRIMINATION
Utah Valley University does not discriminate on the basis of race, color, religion, national origin, sex, sexual orientation, gender identity, gender expression, age (40 and over), disability, veteran status, pregnancy, childbirth, or pregnancy-related conditions, citizenship, genetic information, or other basis protected by applicable law, including Title IX and 34 C.F.R. Part 106, in employment, treatment, admission, access to educational programs and activities, or other University benefits or services. Inquiries about nondiscrimination at UVU may be directed to the U.S. Department of Education’s Office for Civil Rights or UVU’s Title IX Coordinator / Director of Equal Opportunity at 801-863-7999 – [email protected] – 800 W University Pkwy, Orem, 84058, Suite BA 203.
Students shall deliver supervised healthcare services to patients without regard to their race, religion, creed, national origin, sexual orientation, socioeconomic status, disability, disease status, or political beliefs.
RELIGIOUS ACCOMMODATIONS
At the beginning of each semester, the student will have the opportunity to promptly review each course syllabus and class schedule and notify faculty to request an accommodation for sincerely held religious beliefs and practices using the Student Religious Accommodation Request Form.

24
INCLUSION AND DIVERSITY
WHAT WE MEAN BY INCLUSION
UVU is committed to preparing all students and employees for success in an increasingly complex, diverse, and globalized society. We promote civility and respect for the dignity and potential of everyone. We seek to advance the understanding of diverse perspectives. We value and promote collegial relationships and mutual respect among students, faculty, and staff. We acknowledge and seek to address the needs of populations who are underrepresented and students with varying levels of academic preparation, even as we strive to provide access and support for all students and employees in ways that are culturally relevant and responsible.
UVU INCLUSION PLAN
At UVU, include is an action commitment that is a crucial part of our identity. Our dedicated staff, faculty, and students were involved for more than 18 months in constructing Engagement Plan 2024-2028.
UVU PA PROGRAM INCLUSION & DIVERSITY GOALS
HISTORY/COMMITMENT TO DIVERSITY
Inclusion makes students more successful. Over the last several years, UVU has shown itself as a state and national leader in inclusion and diversity efforts, receiving national awards from the White House, Diversity MBA Magazine, and Minority Access Incorporated. As an institution, UVU has chosen to be proactive and far reaching, raising and allocating almost $3.1 million for its inclusion efforts. UVU has 20+ centers, initiatives, and other resources to ensure that students feel safe and championed while attending UVU.
The UVU PA Program has a Diversity Committee that meets regularly to ensure that the environment within the program remains inclusive and that every student has the support they need to succeed. The Diversity Committee advises on program policy, admissions and faculty and staff hiring.

25
ACCOMMODATIONS FOR STUDENTS WITH DISABILITIES
The Office of Accessibility Services (OAS) provides support services for students with disabilities so that they can be successful at UVU. A student who is new to UVU and/or accommodative services can find an outline of the steps to take to determine the accommodations for which they are eligible. The first step is to make an appointment to meet with a counselor in the Office of Accessibility Services. Detailed information can be found at UVU Accessibility Services.
To schedule an appointment to meet with one of the Accessibility Services Counselors, call (801) 863-8747 or visit the Office of Accessibility Services, Business Administration Building (BA-110) Monday-Friday 8am-5pm. Appointments can be scheduled online.
Current UVU students who have not been assessed for learning disabilities are encouraged to meet by appointment with the Office of Accessibility Services (OAS) to discuss off-campus options for assessment. Submitting documentation well before the beginning of the first semester is strongly recommended.
As trainees in a clinical curriculum with direct patient contact, students must meet the technical standards of the program see (Technical Standards Section in this student handbook). All students are entitled to reasonable accommodations for disabilities that are documented, and which do not disqualify the student from meeting competencies described in the technical standards.
Prior accommodations from other institutions are not automatically recognized by the PA program or UVU. All students who seek accommodations must engage with the Office of Accessibility Services to determine if the provision of individual accommodations is possible within the requirements of the PA program. To ensure that students have accommodations in place at the start of each semester, requests for accommodations should be submitted no later than two (2) weeks before the beginning of each semester or as directed by the Office of Accessibility Services.

26
STUDENT MISTREATMENT, DISCRIMINATION, HARASSMENT, AND RETALIATION
A1.02j, A3.15f, A3.15g
POLICIES AND PROCEDURES FOR REPORTING STUDENT MISTREATMENT AND GRIEVANCES:
The medical learning environment is more complex than the undergraduate environment for several reasons. These include:
Effective, caring, and compassionate healthcare depends critically on the professional and collegial attributes acquired by PA students during their education. In this regard, the teacher-student relationship is one of the most important, since the teacher is responsible for both imparting information and guiding the personal development of the student. The teacher also serves as a potential role model for students, and it is therefore important that the teacher’s behavior towards the students is equitable and professional.
Everyone must tolerate the fact that people have different points of view and have the right to speak about those different views. The First Amendment protects most forms of student speech.
At the core of an effective learning environment lies mutual respect between the teacher (including faculty, staff, and preceptors) and the student, and between each student and their student colleagues. UVU will not tolerate harassment or abuse of, discrimination against, or favoritism towards a student by a teacher or a student colleague. Students can reports mistreatment and grievances, see Reporting Misconduct and Behavior Concerns.
UVU EQUITY AND TITLE IX
A3.15g
| UVU Website: | https://www.uvu.edu/equityandtitleix/ |
| Contact: | Title IX Coordinator |
| Email: | [email protected] |
| Telephone: | (801) 863-7999 |
The university is committed to maintaining an inclusive community that values diversity and fosters tolerance and mutual respect. PA students should become familiar with the protections provided by the university regarding to discrimination, harassment, and retaliation. Contact the Office of Equal Opportunity/Title IX for any of the following:
SEXUAL HARASSMENT
A1.02j, A3.15f, A3.15g
UVU’s sexual harassment policy see (Title IX Policies ) applies to students, staff, faculty, and other academic personnel. UVU’s sexual harassment policies help to facilitate an educational environment that is free of sexual violence and harassment while complying with the provisions outlined in the Federal Title IX Act of the 1972 Education Amendments. Sexual harassment is a form of sex discrimination prohibited by Title IX.
IMPERMISSIBLE SEXUAL CONDUCT HARASSMENT INCLUDES THE FOLLOWING
Sexual assault is not an expression of love, passion, or sexual desire. Sexual assault can happen to anyone, regardless of gender, race, class, age, size, appearance, or sexual orientation. Nationwide, alcohol is reported as the most common predatory (date rape) drug in approximately 90% of cases either the victim or the perpetrator was intoxicated. In most cases, the perpetrator is acquainted with the victim.
For further information, see safety, security, and prevention of sexual harassment.
Being assaulted can create a host of practical and emotional consequences. While you may want to talk to someone you trust, such as a friend or family member, there are also confidential campus resources available, including counseling at UVU Student Health Services. UVU’s Student Health Services provides free and highly confidential counseling to students, which can be an extremely important part of the healing process. The Title IX Coordinator can connect you with additional supportive measures and options without any obligation to file a formal complaint or request an investigation. Be advised: university employees other than the counseling staff have an obligation to report instances of prohibited sexual conduct to the Title IX Coordinator. When you seek help from professionals, first ask what level of confidentiality they can provide and to whom they are required to report if you were to disclose information regarding an incident. That way, you can make an informed decision.

27
OFFICE OF THE OMBUDS
A1.02j, A3.15f
Within the UVU community, misunderstandings and disagreements needing resolution may occur. See (Conflict Resolution) for the office of the Ombuds. UVU Ombuds is one who is familiar with campus policies, students' rights and responsibilities, and can help find useful options within these guidelines. To serve as a mediator, as opposed to an advocate, the Ombuds neutrally and objectively listens to all problems. The Ombuds may also help with student grievances. Issues that the Office of the Ombuds can help with are:

28
INTEGRITY IN THE ACADEMIC AND CLINICAL ENVIRONMENT
Since UVU is an academic environment, its fundamental purpose is the sharing and pursuit of knowledge. Imperative to this educational purpose is a commitment to academic integrity. Every member of the UVU community is responsible for always upholding the highest standards of academic integrity. Students are considered integral members of the community and are also expected to adhere to the principles of academic integrity.
Activities that have the effect or intention of interfering with education, pursuit of knowledge, or fair evaluation of a student’s performance are prohibited. Examples of such activities include but are not limited to:
Any violation of the above, whether willful or not, will result in referral to SPC and may result in sanctions up to and including dismissal from the program.

29
ATTENDANCE AND ABSENCES
Didactic Year
It is expected that students are committed to being full-time participants in the program. During the pre-clinical phase of training, it is important for students to be available every day for course activities. While most lectures and workshops are scheduled during the weekday (8:00 a.m. - 5:00 p.m.), students may be required to participate in some weekend, evening, and extended-time curriculum activities. The program will make sincere attempts to give prior notification of changes in schedule. Class schedules cannot be altered to accommodate students who use public transportation or for personal activities/schedules.
Attendance is expected: Students are expected to arrive on time, attend and participate in all program educational activities, including lectures, workshops, case reviews, clinical skills activities, clinical rotations, community assignments, return visits (RVs), examinations (written and practical), and recommended tutorial/remediation activities. Students’ participation in all curriculum activities is expected as part of the academic and professional competencies required for satisfactory progress and professional graduate training.
Students who fail to fully attend and participate in any required activity may not receive full credit for the activity and may be required to complete additional assignments or other activities as assigned by the course director. Students who demonstrate continual, habitual, or excessive absences or late arrivals will be referred to SPC for failure to demonstrate professional behavior. Students who do not correct this behavior will be dismissed from the program.
Students who are unable to attend any scheduled activity must notify the course director in advance detailing any activities or class sessions for which they will not be present. It is the student’s responsibility to arrange the means to get notes or other teaching materials distributed during their absence. Absences that occur during testing events may result in delay in completing requirements and progressing. Students who are ill and miss class or their clinical assignment for two or more consecutive days may be required to submit appropriate medical documentation to the program releasing the student to participate fully in all program activities.
Clinical Year
Students are expected to follow all program reporting instructions, and to notify the program of any errors or changes. An assigned clinical schedule will be determined by the preceptor and should include a minimum of 40 hours per week. Students should anticipate working some evenings, weekends, holidays, or “on call” shifts on various rotations, and must not refuse to work during these times if it is deemed necessary by the preceptor. University holidays do not apply to students’ schedules during the clinical year, and preceptors are not obligated to grant days off to students on holidays or weekends (but may do so at their discretion). Keep in mind that PA students have only one year to receive all their clinical training prior to graduation, so it behooves them to make the most of the time and privilege granted to them of working at clinical sites.
Students will email their clinical rotations schedules (as determined by their preceptor) to the Clinical Education Team by the end of the first week of the rotation. Students must notify the Clinical Education Team as to how they may best be reached during regular office hours, and of any mailing address or phone number changes.
Absenteeism: Adherence to scheduled clinical rotation hours and attendance at all scheduled RVs at the conclusion of rotations are mandatory. Failure to fulfill these requirements is strongly considered in the evaluation of the student’s academic performance and professional attitude and may result in a failing grade for the rotation.
Clinical assignments may require students to drive to sites within a 100-mile radius from the UVU campus. Clinical assignments may require a student to work evenings and extended hours, take call schedules, and participate in on-site activities (e.g. presentations, literature review, written exams, etc.) as assigned by some clinical sites. Students are required to meet these expectations.
If a student must be absent from ONE scheduled clinical rotation shift (this can include any type of shifts), both the preceptor and the Clinical Education Team must be notified as soon as possible. If the appropriate party cannot be reached, then students must leave a phone or electronic message regarding the absence and a phone number where they can be immediately reached.
Students who fail to fully attend and participate in required activity may not receive full credit for the activity and may be required to complete additional assignments or other activities assigned by the course director. Students who demonstrate continual, habitual, or excessive absences or late arrivals will be referred to SPC for failure to demonstrate professional behavior. Students who do not correct this behavior will be dismissed from the program.
Be advised that the program may make random calls and visits to rotation sites to verify student attendance and performance.
Excused Absences: Incapacitating illness, injury requiring bed rest, and unexpected family emergencies are considered valid reasons for absenteeism; however, the procedures for absenteeism as outlined above must be followed. Excused absences greater than TWO (2) scheduled clinical rotation shifts per rotation due to bona fide, documented, medical or personal emergencies may result in a grade of "I" (incomplete) for the rotation. Rotations in which students receive an "I" due to excessive excused absences may be completed later, depending on the availability of the rotation and at the discretion of the Clinical Education Team. For any absence less than the minimum time missed will be made up on an hour for hour basis. Students may request time off, given the policy above, using the Clinical Year Student Time Off Request Form see (Appendix G). Submission of the form does not constitute approval. The form must be submitted 30 days prior to the anticipated absence.
Unexcused Absences and Tardiness: Business appointments, routine dental and doctor appointments, weddings, graduations, family reunions, and other social events are not valid reasons for excused absenteeism. Absenteeism not reported as per policy outlined above will be considered unexcused, regardless of cause or when the program is notified of the event.
Students are expected to always act in a professional manner. Reporting to scheduled clinical work shifts on-time is one of the most important demonstrations of professionalism. Tardiness with rotations and RVs is not acceptable.
Other Situations for Absences: Job interviews are not considered valid reasons for unexcused absences. All attempts must be made to schedule an interview, so it does not interfere with the core clinical. If this cannot be accomplished, students must first obtain permission from the Clinical Education Team to attempt to arrange time off for the interview. Subsequently, the preceptor must grant permission for the absence, and students must make up the missed clinical time within the confines of that rotation. The PA program must be notified as outlined above. A maximum total of TWO (2) days per calendar year will be allowed for interviews.
A “Leave of Absence” may be granted by the program director for extended illness or absence from a rotation. The program director will (on an individual basis) consider emergencies, special requests, and special issues arising that cause students to request a leave of absence, if done prior to failure of the rotation. All student requests are considered private and confidential and are treated as such by the faculty. Absences for scholarly and professional activities will be considered by the clinical education team on a case-by-case basis and must be addressed at least one month prior to the scheduled event.
Inclement Weather: During a weather emergency, student safety is the highest concern. In the event of inclement weather, the program follows the Utah Valley University Snow Days decisions with the following modifications: When the university is closed, didactic classes are canceled. Faculty will notify students of any new arrangements for required activities or exams. The Clinical Education Team will notify students by email of the expectations regarding reporting for clinical duties during inclement weather. As a rule, if you live within walking distance of your clinical site or if you can travel via public transit (assuming it is running), you should report to your site. If you are working at a private practice or another outpatient site, you should call to confirm that the office is open. If travel to the clinical site would be dangerous, students should let their preceptor or site administrator know that they cannot safely travel to the site (you will not be penalized for this decision). If students miss clinical time due to inclement weather, they may be asked to make up this time (especially if the student is on call) if it is feasible within the duty hour restrictions and time left in the clinical rotation.

30
STUDENT SOCIETY AND LEADERSHIP
UVU PA STUDENT SOCIETY
The Utah Valley University Physician Assistant Student Society (UVUPASS) is a registered member of the Student Academy of the American Academy of Physician Assistants (SAAAPA) and is eligible to participate in the American Academy of Physician Assistants (AAPA) National Medical Challenge Bowl, the AAPA Assembly of Representatives (AOR), and the AAPA House of Delegates (HOD).
Members of the UVUPASS participate in a several events in the community and on campus. Students will be responsible for electing class officers who will represent the class. Students will also have a member of the faculty to function as a faculty advisor to the student society.
CLASS RULES
The classroom is the equivalent of a workplace and provides students with the opportunity to practice professional behaviors. Once student leadership is elected for the class, students are encouraged to develop their own “workplace rules” that incorporate and demonstrate the following:
EXTRACURRICULAR ACTIVITIES
While students are encouraged to participate in the many extracurricular activities offered at UVU, they should not miss program curricular activities to participate in extracurricular activities, including UVU-sponsored events or PA professional meetings or activities. Students who are not making satisfactory progress, due to either academic or professional issues, may not hold an office in a student organization or represent the program at university, program, or professional events.

31
CLINICAL YEAR OVERVIEW AND EXPECTATIONS
A3.01, A3.03
The clinical year takes students from the theoretical classroom setting to an active, hands-on learning environment to prepare them for a lifetime of continued refinement of skills and expanded knowledge as a practicing PA. We refer to this clinical experience as a Supervised Clinical Practice Experience (SCPE). To this end, the purpose of the clinical year is to teach the students to:
PREREQUISITES FOR THE CLINICAL YEAR
The clinical year is comprised of the following 10 SCPEs designed to provide clinical experience with preventive, emergent, acute, and chronic patient encounters with patients across the lifespan (infants, children, adolescents, adults, and the elderly). The SCPEs will take place in a combination of the following settings: emergency department, inpatient, outpatient, and the operating room.
*An asterisk indicates a core rotation.
Each SCPE is worth 3 credits and is 4 weeks and 2 days in duration. Students are expected to work at least 40 hours/week according to their preceptor and/or designee’s schedule, possibly including evenings, weekends, and holidays.
CLINICAL SITE PLACEMENTS
A3.03
All clinical sites must be approved, provided, and assigned by the program with an emphasis on an equitable placement for each student. Student preference is taken into consideration but is not guaranteed.
Students will be notified via Exxat of their clinical rotation assignments two to three months in advance of the start of the clinical year. The clinical team will provide additional information unique to each site to help the student transition. Students should reach out to the site prior to the start of the rotation to introduce themselves, express gratitude, and to ensure the first day runs smoothly.
It is NOT the responsibility of the student to provide or solicit sites or preceptors. If desired, a student may suggest a site by completing the Student Clinical Site Request form see (Appendix I) no later than September 30 of the year prior to clinical rotations starting. Each suggested site will be fully vetted by the clinical team to determine if the placement would be appropriate for current and future UVU PA students. There is no guarantee of placement.
REPORTING TO THE SITE
Students must report to clinical sites fully prepared for work with all necessary equipment (i.e. stethoscope, lab coat, identification tag, etc.). Additionally, students are to have the following documents readily available by paper copy and always uploaded to the program student portal in Exxat:
While the program works diligently to monitor the specific requirements of all facilities, frequently facilities will change a protocol without notifying the program. Students are responsible for notifying the program of any protocol changes that they discover, for the program to update the requirements for future students.
ORIENTATION AND COMMUNICATION
Orientation of the student to the rotation site serves several purposes. Orientation facilitates a quicker transition in allowing the student to become a member of the medical team. It also establishes a feeling of enthusiasm and belonging to the team as well as helping students develop the functional capability to work more efficiently.
On the first day of the rotation (or when possible, prior to the rotation), the student should take care of any administrative needs, including obtaining a name badge and computer password, and completing any necessary paperwork, EMR training, and additional site-specific HIPAA training, if needed.
Early in the clinical rotation, it is recommended that the preceptor and student formulate mutual goals regarding what they hope to achieve during the rotation. The preceptor should also communicate his or her expectations of the student during the rotation. Expectations can include:
Students are expected to communicate with preceptors any special scheduling needs they may have during the rotation — in particular, when they may be out of the clinical setting for either personal reasons or program-required educational activities. If students anticipate missing clinical time for personal reasons, they should obtain permission from the program 30 days prior to the clinic absence. See Clinical Year Student Time Off Request Form see (Appendix G)
RESPONSIBILITIES AND DUTIES OF THE STUDENT DURING CLINICAL ROTATIONS
In addition to adhering to the standards of professional conduct outlined in the handbook, students are expected to perform the following during their clinical rotations:
SITE REGULATIONS
A3.01
Students must comply with all rules, regulations, bylaws, and policies of the site for which they are assigned. Failure to do so will result in removal from the rotation and may result in additional disciplinary action. The preceptor or designee will orient the student to the site on the first day. It is the student’s responsibility to ensure they are familiar with the rules, regulations, bylaws, and policies of the site. Program policies must apply to all students, faculty, and staff regardless of location. A signed clinical affiliation agreement or memorandum of understanding may specify that certain program policies will be superseded by those at the clinical site.
RETURN VISITS
Students are required to attend all Return Visits (RV) held after rotations 3, 6, 8, and 10. RVs provide additional opportunities to teach and reinforce critical professional and clinical skills. Completion of the end of rotation examinations and all other activities on the day(s) scheduled by the program is mandatory. Additionally, the capstone and physician assistant practice courses will hold face-to-face classes during RVs. Students must arrive on time for all RV days and stay for the entire day.

32
SAFETY AT THE CLINICAL SITE
Utah Valley University makes every effort to ensure student safety when off campus on clinical rotations through careful vetting of each site and preceptor prior to approval of the site/preceptor for future rotations and annually thereafter through faculty and clinical team evaluations. Additionally, student evaluations of the site provide critical insight about whether the site is safe for future students.
Preceptors are to orient the student to safety measures on the first day of each rotation and students are responsible for following these measures. When a student is participating in a clinical rotation, the university and program recommend that all students be aware of their surroundings at all times and utilize common sense security techniques (i.e. keeping one hand free, locking your car, and concealing valuables from view in your car.) Additionally, the university and program recommend that students utilize any available safety systems present at clinical rotation sites, such as security escorts to your car.
FOR EMERGENCIES CALL 911
If at any time a student does not feel safe in a clinical rotation site, the student is to notify the clinical team immediately. If a crime occurs, students are expected to notify the program immediately, by phone or text to one of the clinical team members, .

33
STUDENT ROLE IN THE CLINICAL SETTING
PATIENT INTERACTIONS
Students must be aware of their limitations as students and of the limitations and regulations pertaining to PA practice. Students at clinical sites must always work under the supervision of a preceptor approved and assigned by the PA program. The students may not function in the place of an employee or assume primary responsibility for a patient’s care. Students must not substitute for or function as instructional faculty or clinical or administrative staff at the clinical site.
Students should always seek advice when appropriate and should not evaluate or treat patients without supervision from, and direct access to, a supervising clinical preceptor. Students will not treat and/or discharge a patient from care without consultation with the clinical preceptor who must assess the patient personally prior to discharge. Such behavior is fraudulent and illegal and may result in disciplinary action. Students will perform only those procedures authorized by the preceptor. Students must adhere to all regulations of the program and the clinical sites. The student is to contact the program immediately with any questions or concerns about the student’s role at a site. Students may not accept monetary or other compensation for services provided during their training.
PRESCRIPTIONS
The preceptor must log into the system under his/her own password and personally sign and send the electronic prescriptions. The student’s name is not to appear on the prescription. These guidelines must not be violated by the student or the preceptor.

34
CLINICAL YEAR EVALUATIONS AND ASSIGNMENTS
It is the student’s responsibility to thoroughly review the syllabus for each SCPE. It is expected that the student is familiar with the learning outcomes, instructional objectives, and corresponding methods of assessment prior to the start of the SCPE. Below is a general description of the assignments and evaluations related to the clinical year.
CLINICAL YEAR PASSPORT
All students will have a clinical year passport to keep track of the expected documentation types, encounters and performance of specific procedures across the clinical year. Documentation, patient encounters and the procedure checklists will be tracked by the student and initialed by the preceptor. Students will review progress on their clinical year passport at each return visit meeting with their advisor. If a student is deficient in achieving clinical year learning outcomes, their rotation schedule may be adjusted. Each student will receive their passport in the clinical year orientation prior to the start of their first rotation. Completion of the passport is required for successful graduation from the program.
EVALUATIONS
ASSIGNMENTS

35
CLINICAL PRECEPTORS
Clinical site preceptors are instructional faculty that have been vetted and approved by the program to be responsible for the clinical education and experience of the student during rotations based on current professional practice. UVU PA preceptors are MDs, DOs, and PAs who hold current board certifications, NCCPA certifications, and licenses that qualify them to practice in their area of instruction.
Preceptors provide guidance, instruction, and oversight to students assigned to their clinical site. Preceptors will review the student’s progress with the student at the mid-point, and submit a written end of rotation evaluation. A student must receive a passing score on the end of rotation preceptor evaluation to pass the SCPE.
Students may not be supervised or evaluated by a resident, faculty member, or other individual who is a family member, or by someone with whom they have had or have a close personal or intimate relationship. While at a clinical site, during their supervised clinical practice experiences, students must not substitute for clinical or administrative staff.
The student should maintain a professional relationship with the preceptor and always adhere to appropriate professional boundaries. Social activities and personal relationships outside of the professional learning environment are inappropriate and could put the student or preceptor in a compromising situation. Contact through social media, except for professional networking sites like LinkedIn and Doximity, should be avoided until the student fully matriculates through the educational program or completes the rotation where the supervision is occurring. If the preceptor and student have an existing personal relationship prior to the start of the rotation, a professional relationship must always be maintained in the clinical setting.

36
TRANSPORTATION AND HOUSING DURING CLINICAL YEAR
All students admitted to the program should expect that they may be placed at remote, underserved, and/or rural clinical sites that are not local to UVU’s campus. The program strives to afford all students the opportunity to work and receive training in a variety of clinical settings. The goal of this is to ensure that students will become well-rounded, culturally/demographically sensitive, and equitable providers. Every effort is made to place students within the UVU service region (Utah, Wasatch, and Summit counties) as well as central and southern Utah in accordance with the program’s mission to strengthen the region’s healthcare workforce. As such, majority of placements will be within 50 miles of the program.
Regardless of placement of clinical rotation, students will continue to be responsible for planning their own living and transportation arrangements. Students are responsible for all parking, transportation, and travel costs incurred during attendance at clinical rotations. Students who attend required rotations and stay in nearby housing are responsible for all costs, risks, and liabilities involved in such housing arrangements. Travel expenses, parking, and housing are not covered by program tuition and will be the student’s personal and financial responsibility to cover and/or arrange.

37
STUDENT IDENTIFICATION
A3.06
Students must be clearly identified in the clinical setting to distinguish them from other health profession students and practitioners. Students must always introduce themselves as a “physician assistant student.” Students should at no time present themselves to patients or other practitioners as a physician, resident, medical student, or as a graduate or certified physician assistant. While at a clinical rotation, students may not use previously earned titles (i.e. RN, MD, DC, PhD, etc.) for identification purposes. Students must wear a clinical jacket with the program identification while at all clinical sites unless instructed not to do so by the clinical site or the program. Students must always wear their program issued identification nametag on clinical sites, in addition to any student identification required by the site. Students must report lost or destroyed nametags within one day and will incur the cost of replacement tags.

38
CONFIDENTIALITY
Students must respect the confidentiality of patients and fellow students. Students must not divulge patient information except to those individuals who have the legal need to know. Students undergo Health Insurance Portability and Accountability Act (HIPAA) training as part of the PA program; training is updated annually. Students must adhere to HIPAA guidelines. Violation of patient confidentiality is one of the most egregious lapses of professionalism, and students who are found to have violated patient trust and confidentiality will face sanctions, which may include counseling, legal charges or fines, suspension, and program dismissal.

39
LIABILITY INSURANCE
Each PA student is covered with liability insurance by UVU through State Risk so long as the students are appropriately engaged in a clinical rotation. Students completing a clinical rotation with a preceptor or site that may end up becoming an employer must maintain a student role in the clinic and should not assume responsibilities of an employee until after graduation from the program. This includes appropriate, routine supervision with the preceptor of record and within the scope of the agreed-upon clinical experience. This is vital in preserving the professional liability coverage provided by the university and is important to protect both the student and the employer in the case that legal action is sought by a patient. Even more critical is the occasional opportunity, or suggestion, from a potential employer to participate in patient-care activities outside of the formal rotation assignment prior to graduation. While these opportunities may be attractive and are seemingly benign, they must be avoided at all costs, as the university’s liability coverage does not cover the student in these circumstances.
In addition, if a PA student is working in a paid position in a different health-care related capacity any time during their PA education, that individual is not permitted to assume the role of a PA student while on duty as a paid employee. Even in a shadowing capacity, it is not appropriate for a student to represent themselves or participate in the care of any patient outside of the role for which they are being paid. Liability insurance will not cover any student assuming the “PA student” role outside of an assigned clinical rotation.

40
INJURY OR EXPOSURE AT CLINICAL SITES
A3.08a,b,c
UVU PA students will participate in clinic both during the didactic and clinical phases through the student-run clinic and through clinical rotations. Prior to participation, all students will be trained in UVU policies addressing student exposure to infectious and environmental hazards, including PPE and bloodborne pathogen training. This training addresses prevention, procedures for care and treatment after exposure, and financial responsibility.
ENVIRONMENTAL HAZARDS (CDC website: Chemical Hazards)
Many hazardous chemicals are present in healthcare settings, which may pose an exposure risk for healthcare workers, patients, and others. These chemicals are used to do the following:
INFECTIOUS HAZARDS (CDC website: Infectious Agents)
Infectious agents are organisms that can produce infection or infectious disease. They include bacteria, fungi, viruses, and parasites. Healthcare workers have a high risk of contact with infectious agents due to the various types of activities involved with their jobs and the possibilities of contamination.
PREVENTION (CDC website: Prevention Controls)
A3.08a
Students are trained in prevention controls outlined by the CDC and NIOSH (see link above), including the use of PPE and ventilation prior to participation in any clinical activity, including the student run clinic during the didactic phase.
PROCEDURES FOR CARE AND TREATMENT AFTER EXPOSURE
A3.08b
The following guidelines address procedures for exposure to bloodborne pathogens and can be generalized to all exposure.
CLINICAL TEAM/FACULTY GUIDELINES
UNIVERSAL PRECAUTIONS
WORKER’S COMPENSATION AND FINANCIAL RESPONSIBILITY FOR TREATING EXPOSURE
A3.08c
Students in clinical settings are considered “interns,” and are therefore, covered under UVU’s Worker Compensation plan. As stated in Utah Code, Unannotated, Volume 3, Title 53, Section 53B- 16-403:
Physician assistant students will be covered under the UVU Workers Compensation Fund policy for medical only if injured during their internship/clinical rotation while working in their scope. The university will not provide additional coverage to physician assistant students beyond the university’s Workers Compensation coverage. As such, physician assistant students are responsible for all other costs and damages associated with exposure to infectious and environmental hazards.
Utah Valley University is insured through its participation in the Risk Management Fund of the State of Utah, see Utah Code 63A-4-101-104, 201. Students are required by the program to maintain health insurance and will be financially responsible for anything not covered as described above.

41
STUDENT EVALUATIONS AND DATA COLLECTION
EVALUATION FORMS
Students are encouraged to complete evaluations on a range of program activities at different points during the program. Evaluations, whether recorded on paper or electronically submitted, are
Evaluations with comments are confidential and are processed anonymously to maintain confidentiality. We value student feedback as an essential part of making our program better.
Feedback is most effective when it is constructive and aimed at helping aspects of teaching and curriculum improve.
DATA COLLECTION FORMS
Requests for data collection come from a range of sources, including the ARC-PA accreditation agency, national and regional PA professional organizations, and governmental agencies that provide student educational grants. The Exxat tracking system is incorporated into the PA program to facilitate data collection. Timely tracking of patient encounters and procedures is a mandatory requirement for successfully completing a rotation. Documentation, including logging patient encounters into Exxat, is part of the student’s rotation grade. Students who do not complete their logging will not get credit for documentation.
The program is required to ensure complete data collection and is accountable for reporting demographic information on each class of students (not as individual data but as grouped, anonymous information).
No personal information is provided by the program to any organizations outside of the university without the individual’s written consent.

42
STUDENT COMPETENCIES
A3.12g
Student evaluation is a continuous process, and multiple methods are employed to determine if a student is making progress in acquiring and expressing competencies specified in the consensus document, Competencies for the Physician Assistant Profession. see (Appendix J)
These Include:
This program is a longitudinal, competency-based, academic program in which students acquire competencies over the course of training in a stepwise, sequential manner. The program's curriculum is designed such that material presented at each phase of training serves as a foundation for subsequent learning and application in clinical activities. Students must satisfactorily complete each component of the curriculum before they continue to the next curriculum phase.
LEARNING EXPECTATIONS
Students are responsible for fulfilling all learning outcomes and instructional objectives. It is not possible nor expected that the student be exposed to each entity or problem listed during their clinical rotation syllabi or that lecturers will discuss all details about each instructional objective; however, it is the student’s responsibility to ensure comprehensive knowledge about all the instructional objectives for each syllabus.
During the clinical phase of education, students must take an active part in the learning process. Active listening skills must be applied to all clinical encounters whether observational or interactive. Students should show initiative and an eagerness to learn. In general, preceptors are likely to invest more time and energy in teaching students who demonstrate significant interest and effort. Students are expected to manage their time well and use slow periods for personal study of program content and preparation for examinations. Students are responsible for all assignments given by the preceptor and the program.

43
METHODS OF EVALUATION
The PA program utilizes various evaluation methods to assess a student’s progress. Methods of evaluation can be defined as formative or summative.
Formative evaluations are given throughout a course to give regular feedback on the student’s progress toward achieving course objectives. The method and frequency of evaluations are described in course syllabi. Course directors, faculty advisors, preceptors, and site visitors work together to provide each student with regular feedback on his/her progress and include remedial recommendations or requirements for strengthening academic and professional competencies.
Summative evaluations are conducted in most courses to assess cumulative learning and contribute to the determination of a course grade. Methods of evaluation and requirements to pass are described in the syllabus for each course. These are structured and weighted to indicate that a student has retained and mastered concepts throughout the course.
Formative and summative methods may include but are not limited to:
Examinations are the sole property of the UVU PA Program. Students should see their specific course syllabi for assessment and grading methods. In line with university policies, students may not be evaluated (for example: OSCE, clinical rotation performance) by a family member or by someone with whom they have or have had a close personal or intimate relationship. Copies, results, or summaries of evaluations may be maintained in the student’s academic file.

44
END-OF-PROGRAM SUMMATIVE
B4.03a-e
The comprehensive Summative Evaluation is a mandatory graduation requirement see (Graduation Requirements) administered in March, approximately eight weeks before the end of the program, to verify that every student meets the competencies necessary for entry into clinical practice. The Summative Evaluation is introduced to the students in the first week of the program and then again in the first week of the last semester. Students can ask questions about the summative at any time. This evaluation assesses the student's mastery across the program's seven competency areas and aligns with the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA) standards. The comprehensive Summative Evaluation is comprised of three parts:
The PAEA End of Curriculum Exam is the written portion of the summative evaluation and is designed to objectively assess the student’s core medical knowledge, specifically focusing on the program competency area of “Knowledge for Practice.”
· Structure: A standardized, multiple -choice examination reflecting knowledge gained across the entire PA program curriculum, mapped to the NCCPA PANCE blueprint. This is a 300-question exam. PAEA End of Curriculum info
· Passing Score: Students must achieve a score of 1450 or higher.
· Remediation: Students who fail are required to complete specific content modules within four weeks. They are granted one re-examination opportunity. If the student fails the second written examination, they will be referred to the Student Progress Committee (SPC) for review.
The OSCE stations serve as the practical portion of the summative evaluation and is designed to evaluate the student’s ability to apply medical knowledge, clinical and technical skills, and appropriate professional behaviors within simulated patient encounters. It assesses several program competencies, including Knowledge for Practice, Interpersonal and Communication Skills, Person Centered care, Professionalism and Ethics, and Society and Population Health.
· Structure: A 6-station OSCE-style exam using diverse standardized patients. Proficiencies evaluated include patient history and physical examination, ordering and interpreting diagnostic tests, clinical/technical skills, oral case presentation, appropriate documentation (including use of information technology and resources), evaluation of medical literature, and overall professionalism.
· Passing Score: Students must pass each OSCE station of the exam with 75% or higher.
· Remediation: Failure of this portion requires the student to meet with a faculty mentor to develop a focused remediation plan based on identified deficiencies. Remediation must be completed within four weeks, followed by a re-examination. If the student fails the second practical exam, they will be referred to the Student Progress Committee.
The Quality Improvement (QI) Presentation portion of the summative evaluation assesses the program competency “Practice-based Learning and Quality Improvement”.
· Structure: Students present a quality improvement project derived from their supervised clinical practice experiences. The presentation is graded using a rubric that evaluates the student’s understanding of QI concepts
· Passing Score: Students must receive 75% or higher.
· Remediation: Students who do not pass meet with a faculty mentor to develop a specific remediation plan. They are given one opportunity to give the presentation again in four weeks. Failure on the second attempt results in a referral to the Student Progress Committee.
Remediation and Progression Policy
If a student fails to pass the second attempt of any summative section, they will be referred to the Student Progress Committee (SPC). The SPC reviews the case to determine appropriate action, which may include recommending an extension of the course of study, requiring further remediation, or considering possible program dismissal.

45
ACADEMIC STANDARDS AND DEADLINES
A3.15a, A3.15b
GLOSSARY OF TERMS:
Intervention: The act of intervening. In education, this would generally involve a faculty-directed activity to help a student achieve a successful outcome.
Retesting: An opportunity to demonstrate proficiency or meet a benchmark without formal remediation.
Formal Remediation: A formal action taken to correct professionalism or academic deficiencies that would otherwise prevent a student’s progression in the program. Requires documentation via a learning contract.
Probation: A status or time when a student is undergoing remediation to correct professionalism and/or academic performance and during which consequences of failing to meet expectations are agreed upon.
Deceleration: A decision made by the Student Progress Committee to delay a student’s progress. During the didactic year, this will result in the student taking a leave of absence and rejoining the next cohort at the beginning of the corresponding semester in which the student initiated the leave of absence (if initiated in the spring semester, will rejoin the following spring semester).
Dismissal: Removal of a student from the program for professionalism or academic deficiencies.
Leave of Absence: A temporary cessation of study for medical reasons or other emergencies up to one year. Requires submission of appropriate form to the program director.
Withdrawal: Ceasing study within the physician assistant program by the student’s request and complying with withdrawal policies as spelled out in UVU student rights. Requires a petition to withdraw per UVU Student’s Rights and Responsibilities. Withdrawal from an individual course may not allow a student to progress in the program as per the requirements for progression and therefore may constitute withdrawal from the program.
Academic Deficiency: Failure to meet an academic benchmark in one or more courses/summative assessments or professional misconduct.
Student Learning Contract See (Appendix K): An agreement between a student and an assigned faculty member or the Student Progress Committee that explains requirements to correct academic or professionalism deficiencies and consequences of not completing remediation.
Professional Misconduct: Failure to behave in a professional and respectful manner as defined by the program.
Informal Incident Report: A written warning to the student about professional misconduct that was reported to the Student Progress Committee by faculty, staff, preceptors, or students.
Formal Incident Report See (Appendix L):A written notification from the Student Progress Committee to the student indicating professional misconduct that warrants probation and outlines a formal remediation plan or SPC decision on student status.
PROGRAM COMPLETION DEADLINES AND REQUIREMENTS
Due to the sequential nature of the curriculum, students must successfully complete all courses for a given semester to be eligible to enroll in courses in the subsequent semester. Students must successfully complete all courses in the didactic phase before they may progress into the clinical phase of the program. The maximum amount of time allowed to complete all program requirements is 39 months. To participate in graduation, students must be scheduled to complete coursework within 12 weeks of graduation date.
Supervised clinical practice experiences offered during the clinical phase of the program do not follow the semester calendar. Due to timing, as well as complexity of evaluative measures incorporated, student performance is assessed at the completion of each Supervised Clinical Practice Experience to determine progression to the next rotation.
EXPECTED PROGRESSION OF THE PA STUDENT
Students on clinical rotations will build on the didactic training and foundations to take detailed histories, perform physical examinations, give oral presentations of patient findings to the preceptor, and develop differential diagnoses. As the year continues, the student should be able to more effectively come up with an assessment and plan, though this will involve discussion with the preceptor. If the preceptor deems it necessary, students initially may observe patient encounters. However, by the end of the first week, students should actively participate in evaluating patients. As the student hones their skills and abilities and discusses this with the preceptor, there should be enough student progress for the preceptor to feel comfortable in allowing progressively increasing supervised autonomy.
At the conclusion of each semester, the Student Progress Committee (SPC) reviews each student’s academic and professional performance. Students must be recommended for progression by the SPC to be eligible to take courses in the subsequent semester and continue their progression through the program. At any time, a student is identified as at risk for academic deficiency, the SPC may convene to determine an appropriate action.
Students remediating a course or course component may progress to the subsequent semester at the discretion of the SPC.
If a student fails to meet the guidelines of satisfactory progress in a course, the following may occur depending on when the deficiency is identified:
When academic deficiency is identified:
ACADEMIC STANDARDS (Course Failure, GPA <3.0 and Professional Misconduct)
Despite efforts to remediate deficits, a student may earn a course grade less than a C.
DIDACTIC YEAR TEST REMEDIATION POLICY
CLINICAL YEAR TEST REMEDIATION POLICY
PROFESSIONAL MISCONDUCT
Expectations for professional conduct of UVU PA students can be found in the ‘Professional Conduct’ section (Section 19) of the student handbook.
Informal incident reports are not filed in the student’s permanent file unless the issue escalates; they then may become formal incident reports that are placed in the student’s permanent file. Formal incident reports result in academic probation or dismissal.

46
STUDENT PROGRESS COMMITTEE
THE PRIMARY CHARGES OF THE SPC ARE TO:
The SPC is composed of the chair, co-chair, full-time principal faculty members, and medical directors. The program director functions as part of the appeals process and therefore does not serve on the SPC.
The SPC intervenes with “at-risk” students to identify issues that may affect a student’s ability to make satisfactory academic or professional progress. Students will be notified in writing as to the date, time, and purpose of required SPC meetings they are expected to attend. During the meeting, students may rebut any items initiating the action and present relevant information that substantiates their position.
The SPC process is as follows:

47
ACADEMIC PROBATION
A3.15c
The process of probation is as follows:
If a student refuses to sign the letter with the terms of probation, the student must submit a letter of appeal to the program director within ten (10) business days from the date that the probation letter was received. If not submitted within this time frame, the student will be held accountable for all of the terms as outlined. During this appeal process, the student may be prevented from participating in program activities.
NOTE: Students on probation may not serve on extracurricular committees, be assigned to clinical rotations outside of a 60-mile radius of the program, and may not serve as a student officer on student committees, organizations, or societies. These students may not participate in the applicant interview process and may not represent the program at profession-related events (e.g., AAPA, CAPA, PAEA, and health fairs).

48
DISMISSAL
A3.15d
Students may be dismissed from the program without first having been placed on probation for either academic or professional misconduct issues. Professional misconduct may constitute the sole reason for dismissal from the program.
Dismissal from the PA program is the result of failure to achieve academic grades and/or demonstrate competencies required of all students. Dismissal could occur after unsuccessful efforts at remediating or appealing course grades as described above or for professional issues. Violations of PA and university codes of conduct, technical standards, or community laws may also result in dismissal. The process is described as follows:

49
APPEALS
A3.15g
APPEALS OF PROGRAM DECISIONS REGARDING STUDENT PROGRESS (other than dismissal)
Students have the right to appeal decisions made by the SPC and program director but must do so in the prescribed stepwise administrative process described below. A department advisor/ombudsperson will assist the student in understanding the steps of the appeal process.
A student may challenge an academic sanction as provided in UVU Policy 548 Academic Rights and Responsibilities of Healthcare and Counseling Clinical Program Students. The reason for appeal must include not just the student’s disagreement with the sanction, but that the sanction is “arbitrary or capricious,” as defined in UVU Policy 548.
When receiving notice of academic sanction from the SPC, students will receive instructions on how to appeal consistent with UVU Policy 548, including where to send their appeal and deadlines for appealing.
During the appeals process, the student may be prevented from participating in program activities, particularly those appealing a dismissal.
If a student wishes to challenge an academic sanction as unlawful discrimination, the complaint process for such a claim is administered by the Equity & Title IX Office and is described in UVU Policy 165 Discrimination and Harassment.
APPEALING A COURSE GRADE OR OTHER PROGRAM EVALUATION
Once a course grade is determined by the course director or faculty of record, students can appeal the grade only through the process outlined in UVU Policy 523 Grading Policy. This process begins with an informal consultation with the instructor, and the steps below describing that informal consultation in more detail. If a resolution cannot be reached at this informal stage, the student may then advance the appeal to the university level.
The following steps are meant to provide guidance to students endeavoring to resolve grade disputes at the department level.
This PA department-level appeal process must be completed before the beginning of the next semester. An unsuccessful appeal at the department level will result in the student being prohibited from progressing to the next semester. The student will be referred to SPC for further action. A student may wish to initiate a university review as soon as the departmental resolution to the dispute has failed. The process for appealing a final course grade is described in Section 5.4 of UVU Policy 523 Grading Policy.
All relevant documents and communication. will be retained by the chair of SPC.

50
LEAVE OF ABSENCE
Interruptions of enrollment can cause problems in the continuity of coursework within a professional graduate program and therefore, leaves of absence are generally discouraged and may impact the student’s ability to progress within the standard program timeline. Interruption of studies may only be done for compelling reasons (e.g., maternity/paternity leave, sustained ill health, and extraordinary personal issues). Students requesting a leave of absence must submit a Graduate Student Leave of Absence Request form and meet with the program director.
All graduate students must complete the Graduate Student Leave of Absence form and have it approved by the program director and the UVU Director of Graduate Studies if seeking to take a leave of absence from their studies. Contact the Graduate Studies Office at 801-863-8097 with any questions.
The procedure for requesting a leave of absence is different depending on the reason for the leave:
A student must be in “good standing” and making satisfactory progress to request a leave of absence. Interruption of studies may only be requested for a compelling reason. The student must petition a leave of absence for a stated period. Students who find it necessary to be excused from registration must request a leave of absence by the last day of registration to drop or add courses. The request should include a timeline for the students' return.
A student who does not return to enrolled status at the end of an approved period of a leave of absence is no longer considered to be pursuing an advanced degree. Students who fail to apply for a leave of absence or for whom a leave of absence has been denied (or has expired) are subject to policies governing continuous enrollment and readmission.
For additional information and possible outcomes, please refer to the following information on the Graduate Studies website.

51
READMISSION AND RETURNING FROM A LEAVE OF ABSENCE
Readmission
A student who leaves the university without obtaining a formal leave of absence from graduate studies is not automatically readmitted. A student wishing to apply for readmission to the physician assistant program must reapply in the next admissions cycle.
Leave of Absence
When a student on official leave of absence is ready to return to the program, the student must give the program director advanced notice in writing to initiate the re-entry process. Students must submit a letter of intent to return to the program director at least ten (10) business days prior to their expected return or as outlined in the original approval letter. Failure to follow this process may result in the student’s delay in expected progression through the program.
All students returning from leave of absence will be required to meet with either the program director or the SPC to ensure that they can meet the technical standards of the program, and to determine if they are eligible for continuation of their training.
Students who have taken a leave of significant length may be required to repeat some parts of the program or the entire program, as well as any remediation activities determined by the SPC before resuming their original position within the program. Students returning from a leave during their clinical phase of training may be required to repeat some or all their course activities. Whether a student has a clinical assignment immediately available to them, when they are ready to return to active student status, depends on the availability of clinical training sites.
Students should be aware that successfully completed courses may not be repeated for credit. Any coursework or clinical instruction deemed appropriate by the SPC for the student to retake to return to an appropriate level of progression may require the student to audit courses without credit. Since university registration is required for this process, the student must be willing to bear both the time and financial consequences.
A student who is granted leave of absence is expected to complete all the coursework missed and/or courses. If the leave of absence will disrupt the completion of didactic courses in which the student is enrolled, the student may be required to decelerate. The requirements to return after a leave of absence must be concluded within a twelve (12) month time frame. A leave of absence is permitted only ONCE during the didactic year. The longest a student may take to complete the program is a 39-month time frame. Any leave of absence, deceleration or remediation must be completed within a (12) month time frame.

52
DECELERATION
A3.15c
Deceleration is any disruption in the student's progress due to academic deficiency that will extend the date of graduation beyond that of his/her cohort. The length of deceleration will be determined by the SPC if it is part of a remediation plan or studentlearning contract. Upon deceleration, the student will be required to demonstrate competency upon return to the program. This could be in the form of a written comprehensive examination, practical examination, retaking previously passed courses and/or participating in a student learning contract while on leave. The type of assessment will be determined on a case-by-case basis. Because courses in the physician assistant program are offered only once per academic year and serve as prerequisites for subsequent courses, deceleration typically lasts for one year during the didactic curriculum. The requirements to prove competency after deceleration must be concluded within a twelve (12) month time frame. A leave of absence or deceleration is permitted only ONCE during the didactic year. The longest a student may take to complete the program is a 39-month time frame. Any leave of absence, deceleration or remediation must be completed within a (12) month time frame.

53
WITHDRAWAL
A3.15d
Students are permitted to withdraw from the program at their discretion following the university defined procedure in UVU Policy #503 Add/Drop/Withdraw and complete appropriate forms.
Withdrawal from an individual course will not allow a student to progress in the program as per the requirements for progression and may therefore constitute a withdrawal from the program.
To officially withdraw from the university, a student must report to the UVU Registrar’s Office. Students wishing to withdraw should also consult with the Office of Student Financial Aid to determine if stipulations associated with the financial aid package will lead to changes in the financial statement.
You can officially withdraw from a course by dropping it through the online registration system by the listed date. If you officially withdraw from a course by the "Last Day to Drop and Not Show on Transcript," the course will not appear on your academic transcripts. If you officially withdraw from a course by the "Last Day to Withdraw," a "W" will appear on your transcripts. Although your GPA will not be affected — a "W" will indicate that you chose to withdraw. If you fail to complete the course and do not drop it before the "Last Day to Withdraw," a "UW" or "E" (a failing grade) will appear on your transcripts.
Withdrawing from a course may impact your financial aid status. For more information, see (UVU Financial and Scholarships Aid).
LATE WITHDRAWAL PETITIONS
This provides an opportunity for students to petition the registrar and department chairs for a withdrawal, based on extenuating circumstances occurring after the established withdrawal deadlines. These are considered exceptions to the withdrawal policy.
POLICIES AND GUIDELINES
Students who find themselves in extenuating circumstances beyond their own control that prohibit attendance or participation in currently registered classes may petition through the UVU Registrar's Office for withdrawal.
See (UVU Petitions)

54
SAFETY AND EMERGENCY MANAGEMENT
*IN AN EMERGENCY DIAL 911*
IMPORTANT NUMBERS AND RESOURCES
| UVU Department | URL | Phone |
| Police | https://www.uvu.edu/police/ | 801-863-5555 |
| Emergency Management | https://www.uvu.edu/emergencymanagement/ | 801-863-7977 |
| Emergency Information | https://www.uvu.info/ | 801-863-INFO (4636) |
| Student Health Services | https://www.uvu.edu/studenthealth/ | 801-863-8876 |
| Facilities & Planning | https://www.uvu.edu/facilities/ | 801-863-8130 |
| Office of Risk Management | https://www.uvu.edu/riskmanagement/ | 801-863-5973 |
| Environmental Health & Safety | https://www.uvu.edu/safety/health/ | 801-863-8560 |

55
STUDENT SERVICES
UVU Fulton Library
The UVU Fulton Library provides all PA students with initial “one-stop-shopping” for articles/books/videos relating to PA research, and provides access to online journals, textbooks, and medical search engines. UVU Fulton Library offers access to a vast collection of academic textbook titles, eBook titles appropriate for PA students, streamed medical education videos, periodical databases, peer-reviewed journal titles, full text for many of the CINAHL journals, PubMed, Science Direct Journals, Cochrane Library collection, Web of Science, PsycInfo, PsycARTICLES, JSTOR, Oxford Reference Online, Alt-Health Watch, and many more resources that come highly recommended for PA students and faculty.
Collections housed in R areas of the Library of Congress classification system include PA subject areas such as general medicine, public aspects of medicine, pathology, epidemiology, pediatrics, gynecology, diseases, pharmacology and so forth. The library specialist assigned to health sciences will work with the PA department to augment the current collection as needed.
All library users have direct access to the ILLiad interlibrary loan system. Most items are delivered electronically, via email. If there is demand for returnable ILL items (i.e., books) at the remote site, UVU will investigate establishing an ILL courier service to serve the site.
The library’s home page serves as the gateway to information resources and services. Internet access provides students and faculty at off-campus and remote sites immediate, transparent access to all the library’s electronic materials. See (Fulton Library).
Campus librarians are available to support students and faculty by both face-to-face and virtual consultations. The library reference desk can be accessed through popular instant-messaging programs, text messages by phone or through the campus communications Outlook-based platforms, via e-mail, or in person. Students and staff may also make individual face-to-face or telephone appointments with subject specialists for more in-depth assistance with their research.
A specific subject-area specialist will be assigned to the PA program. This librarian will serve as the primary library contact for PA students and faculty members, and will support culminating experience projects, capstones and other in-depth research projects.
For current information about library hours, including reference service hours, please see library services here. Students will have electronic access to all digital library information resources.
UVU BOOKSTORE
The UVU Bookstore is the official store of Utah Valley University and is located on the UVU main campus in SC 102. Check the bookstore website for hours. For information, students can access the Official Store of Utah Valley University here.
Students can purchase textbooks via UVU Online Bookstore and have the option to ship their textbooks to either their home or to a designated on-campus location. Textbooks are not available at the UVU bookstore.
PARKING
All vehicles parked on campus require a parking permit
We anticipate significant parking and traffic congestion at the beginning of each semester. Here are some suggestions that may help to lessen the impact of parking issues:
Contact the Parking Office at (801) 863-8188, if you have any questions.
FINANCIAL AID
Students are responsible for obtaining their own financial aid. The program is not involved in the process of granting financial aid except to respond to requests from lending institutions for specific documentation such as student enrollment, academic schedule, and expected date of graduation.
The Financial Aid Office is located on the UVU main campus. The Financial Aid Office is responsible for assessing student eligibility for financial aid. The staff is also available to counsel students on the most appropriate and available resources to meet individual needs. The Financial Aid Office manages and distributes a limited number of scholarships for eligible students. Financial aid is granted based on both federal and university guidelines.
Students requiring financial assistance are encouraged to seek loan counseling and assistance in debt management before making any financial decisions. Since the application process is lengthy and often complex, it is suggested that students apply early for FAFSA and financial aid each year. Students can find additional information about financial aid. See (UVU Financial Aid & Scholarships).
UVU STUDENT HEALTH and WELLNESS SERVICES
All PA students are eligible to receive basic health services through UVU’s Student Health Services which offers traditional medical services, mental health services, learning disability assessment, psychiatric services, and suicide awareness and prevention. Students have access to Student Health Services on Monday, Wednesday, Thursday from 8am - 7pm and Tuesday, Friday from 8am - 5pm. See (Student Health Services).
As a division of the student health center, the crisis center offers services to help students deal with urgent mental health issues and other issues surrounding mental health. If a student is in crisis, that student can call for an appointment at UVU Student Health Services (801) 863-8876, M-F 8am-5pm), and notify the person answering the phone that this is an emergency for priority scheduling.
Other resources available for any student in crisis mode:
IN CASE OF EMERGENCY
Call one of the following:
The Student Life and Wellness Center works to support students by offering a variety of life and health enhancing services that increase safety, productivity, and life experience of the individual and the campus. More information is available about these programs and activities. See (StudentLife & Wellness Center).

56
PA PROFESSIONAL RESOURCES
The following resources are available about PAs, related programs, and for practicing PAs:
U.S. Bureau of Labor Statistics - Physician Assistant
Student Academy of the American Academy of Physician Assistants (SAAAPA)
American Academy of Physician Assistants (AAPA)
Utah Academy of Physician Assistants (UAPA)
Physician Assistant Foundation
Accreditation Review Commission on Education for the Physician Assistant (ARC-PA)
National Commission on Certification of Physician Assistants (NCCPA)

57
APPENDICES