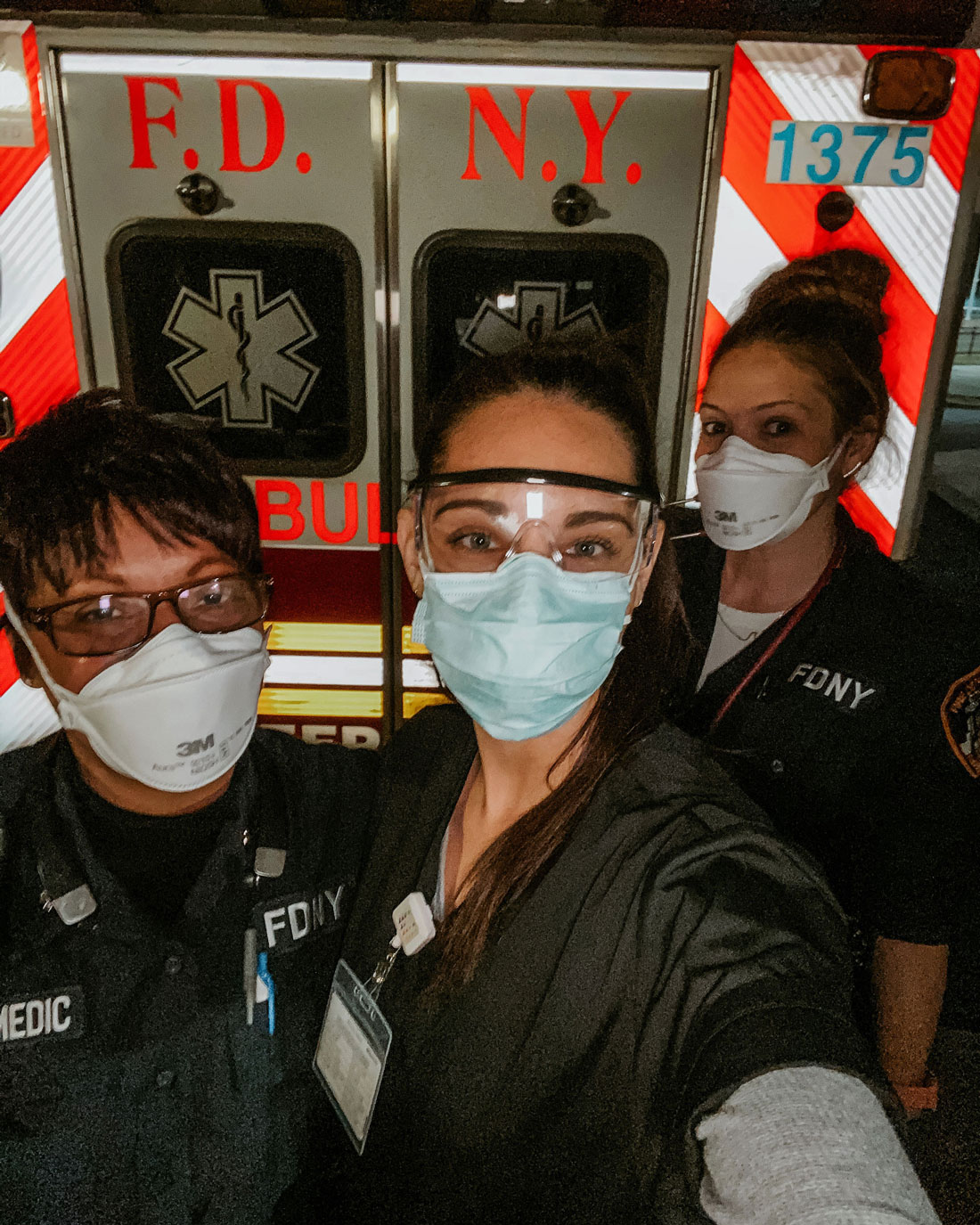
Pictured: Intermountain Healthcare Crisis Response Team deployed in New York. Center: Krystal Lazenby

One of the core values of Utah Valley University is “exceptional care.” But the COVID-19 pandemic has made it challenging for many to show that care in their usual ways.
That’s been true of UVU grads and students studying and working in medical professions, too. They’ve had to learn and adapt quickly to the realities of a virus that has stumped experts and changed the normal expectations of medical care. But they’ve risen to the challenge.
UVU Magazine reached out to several of these Wolverines to find out what it feels like on the front lines of a global pandemic. Here’s what they told us.
By UVU Magazine Staff | Photography by Staff and Nurses

Pictured from Left to right:
Amanda Cook, Lindsey Porter, Kalin Hofheins
Krystal Lazenby
Hometown: Salem, Utah
UVU nursing graduate
In April I was fortunate to be picked as part of the Intermountain Healthcare Crisis Response Team to deploy to New York for 16 days to assist with the overwhelming number of patients who tested positive for COVID-19. I was stationed in the emergency room of Long Island Jewish Medical Center.
It was difficult to see patients so sick, scared, and all alone because family members weren’t allowed in the hospital at that time. On the floors, two medical or surgical patients were placed in rooms meant for only one patient. In the ICUs, patients were packed in like sardines — all lined up, intubated, beds only far enough apart for one nurse or other healthcare team member to work on their patient. It was heartbreaking and grim, knowing the statistics of the mortality rate and that the majority of them would not be going home.
The frontline workers of New York are truly heroes. They have been working so hard, some of them with only a day or two off during the weeks of the peak. Everyone who found out we were there from out of state was so incredibly grateful for answering their call for help. They were exhausted, mentally and physically, and still continue to show up, day after day.
The UVU nursing program has always had a fantastic reputation, and they completely lived up to it. The instructors help create a solid foundation to build upon as a nurse. I am always so proud to say I am a Wolverine.
Amanda Cook
Hometown: West Jordan, Utah
UVU nursing graduate
During COVID-19, I have been working on the Respiratory and Sepsis Unit at Utah Valley Hospital.
The most difficult thing is being so precise about entering and exiting rooms of COVID patients. This is because we want to contain the virus, not getting it ourselves or spreading it to other patients or coworkers. It is hard to have to wear so much isolation all the time, mostly because it is uncomfortable, but it also takes time. It is also really difficult to see COVID-19 patients and how sick they are but not be able to have any visitors. They also have very limited interaction with hospital staff, so they are basically in a room that they can’t come out of and all alone. It is hard to watch, and a lot of them have a hard time.
The most rewarding thing is seeing these patients recover and get to go home to their families.
At UVU, we learned a lot about patient interaction — I feel like that was so important in this situation because there are a lot of the hospital staff that can’t go in the rooms and have to do their jobs over the phone. This makes human interaction with the patients very slim, so the interaction experience they do get is important.
With COVID-19, a patient’s condition can change rapidly, and I have really appreciated knowing how to be flexible and adapt to different situations.
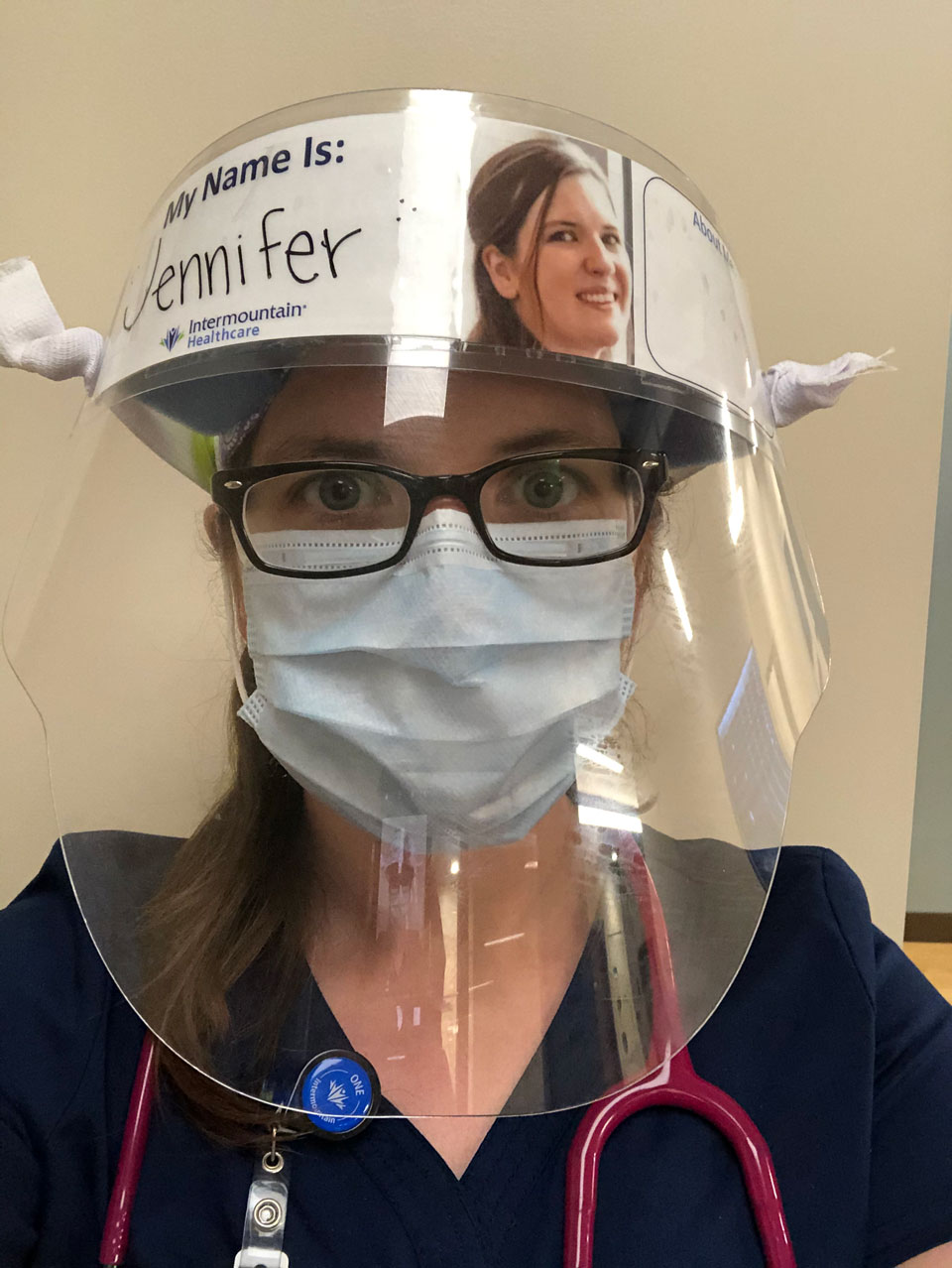
Pictured: Jennifer Salazar
“I started working in January, so I am already trying to learn how the hospital as
a whole works, but now I am also learning how to operate during a pandemic.”
– Jennifer Salazar
“The frontline workers of New York are truly heroes.”
– Krystal Lazenby
“Keeping to a routine has helped me with the pandemic's challenges.”
– Sierra Webb
Jennifer Salazar
Hometown: Moravia, New York
UVU nursing student
I work as a nurse at Utah Valley Hospital. I don't work directly with COVID-19 patients, but I test those who we are going to discharge to a nursing facility. I started working in January, so I am already trying to learn how the hospital as a whole works, but now I am also learning how to operate during a pandemic.
Coming home after work is difficult. I have three kids, and it's hard on them to have me be at work for 12-plus hours a day. They want to run up and hug me as soon as I walk in the door. Before I let them do that, I have to carefully change out of my scrubs, take a shower, and disinfect everything I brought with me — keys, lunch bag, name tag, phone, and shoes. Sometimes getting clean enough to see them takes another 30 minutes. I am constantly worried about bringing home diseases to my family.
The biggest thing I learned from my time at UVU is time management. UVU’s program teaches us how to lump care together and, most importantly, how to delegate tasks. This is important as a nurse in general, but it is very important now.
To the public, I would say: Try to be patient with us. We are trying to do everything we can to keep our patients safe and prevent the spread of COVID-19, but we are still learning what that is. Stay home, wear a mask, wash your hands, and continue to practice social distancing.


Pictured: Dani Thornton, RN, BSN wearing a variety of personal protective equipment.
Sierra Webb
Hometown: American Fork, Utah
UVU nursing student
During the COVID-19 pandemic, I have been working as a medical-surgical nurse on the COVID-19 unit. I have been providing bedside care to those who have been tested for COVID or have positive COVID results and need extra help at the hospital.
Keeping to a routine has helped me with the pandemic’s challenges. The most difficult thing about working during COVID-19 is all of the policy changes that change hourly. It felt like we were never on top of the newest changes, and people had heard different things from different leaders. Our manager would send out videos daily to make sure we were up to date on the latest, but even those “up-to-date” statuses changed quickly, sometimes during a shift. So we have had to adapt to change.
The most rewarding thing about working during COVID-19 is knowing that I am saving lives by going to work. I love to see my patients improve. I also love to educate them. There are a lot of unknowns about COVID-19. But the small information that we did know, I was able to educate my patients on.
It also helped that the world recognized my efforts. I think that being a nurse during COVID-19 would be a lot harder without the support from the community.
Brianne Cole
Hometown: Midwest City, Oklahoma
UVU adjunct professor
I work at Jordan Valley Medical Center in the Labor and Delivery Unit.
The most difficult thing about working with COVID-19 patients is the uncertainty. As a nursing professor and 10-year veteran of the profession, I'm accustomed to knowing the answers. This pandemic has busted us all back to beginners. Even our experts are helplessly unsure of how to best protect ourselves and our patients.
I'm drawing on lessons I've learned from my students: how to be patient, to discern the best course of action from conflicting information, to accept correction with grace, to rapidly assimilate and effectively utilize novel information, and to do the best I can with what I have.
The most rewarding thing so far has been the gratitude of the patients. One of the people I took care of compared her experience to the HIV/AIDS epidemic: people were scared to touch others, to hug them, to even be in the same room with them. I've had patients thank me for not being scared to take care of them. I'm terrified, naturally, but that is the nature of professionalism in healthcare — to put the good of those who are vulnerable first. The gratitude of frightened people for simple human care has been humbling.
I would like the public to know that if you're sick, it doesn't matter. We'll still do our very best to try to assure your return to health. We're afraid, of course, but it's not going to stop us from jumping in to save you. Just please, be patient with us. We are students again, and we're doing our best — but we're still learning.
Jared Brooksby
Hometown: West Jordan, Utah
UVU biotechnology graduate
I work at BioFire Diagnostics. We make rapid molecular tests for syndromic diagnostics of infectious diseases. Most recently, we have received emergency use authorization for the BioFire Respiratory Panel 2.1, which tests for the SARS-CoV-2 virus as well as 21 other common respiratory pathogens.
The most difficult thing about working during this pandemic has been the speed at which we have had to work to release our test and to ensure that we have created a quality product. When you are working on an accelerated timeline and there are setbacks, you have to find ways to quickly overcome them without being discouraged.
The most rewarding thing is knowing that what we develop will directly help in saving lives. We know our tests are generally used in hospitals and reserved for those patients who are the most sick. It could be the difference in giving someone the correct treatment possibly days earlier than they would have received otherwise.
UVU taught me the technical skills of working in a lab. My biotech, microbiology, and molecular biology classes taught me what I needed to know to work with live pathogens and with the tests prominently used for diagnosing SARS-CoV-2.
I think that people should know that companies continue developing and improving testing for COVID-19. We understand how much of an impact appropriate testing will have on the course of this pandemic and on so many individual lives. We hope that everyone will take this disease seriously and will support all medical personnel involved in treating those who are sick.
“After watching someone not do anything for over a month, and then one day finally
be able to get off the ventilator, and eventually eat, and start talking again, then
be able to leave — that's amazing.”
– Dylan Richmond

Pictured: Dylan Richmond
Dylan Richmond
Hometown: Blanding, Utah
UVU nursing graduate
I took a job in New York to help with the crazy numbers that they have seen. I've been working in a COVID-19 ICU since the very start of April. The patients I see are very, very sick. The hardest thing for me is that I've had a few 35-year-old patients — with no underlying conditions — who have been the most sick. Watching those patients progress until they go into multi-organ failure is the worst.
The most rewarding thing is that we have had a few ICU patients leave. After watching someone not do anything for over a month, and then one day finally be able to get off of the ventilator, and eventually eat, and start talking again, then be able to leave — that’s amazing.
The nursing program at UVU taught us how to be truly compassionate caregivers and advocate for our patients always.

Pictured from left to right:
Sierra Webb, Danielle Bennett, Brianne Cole

Pictured: Krystal Lazenby
Veronica Martinez
Hometown: Chicago, Illinois
UVU biotechnology student
I didn't understand the severity of the virus until I physically had a patient make their way to the emergency room gasping for air. They couldn't breathe well, and their whole family had tested positive. I personally took the patient into quarantine to make sure he didn't lose consciousness on the way.
That night, I went home and slept in our guest room while my husband slept in our bedroom. I awaited a phone call from my boss to be granted permission to return to work again. Shortly after, we were advised to monitor our temperatures twice a day and continue on in the pandemic.
The fear of not knowing if I was a carrier was the worst part for me. We go into work daily not knowing what diseases we may come in contact with, so infection prevention and standard precautions are part of our everyday life. Even so, I still had a lot of exposure. I didn't leave the house after work. It wasn't about me getting sick — it was about who I could pass it to that may not be able to fight as hard.
The best part was experiencing emergency medicine, the adrenaline rush of helping patients of all ages and all different ailments. We were one of the first to know of changes, new symptoms, and preventative measures. The community members supported us by staying home or catering food. It was a new kind of love and assurance.
One of the many reasons I love UVU is because you can express yourself in the way that feels best, and you're always accepted for it. It's safe ground. In the medical field, you meet all kinds of people who trust you and tell you their secrets. The vulnerability between patient and caregiver is special — another kind of safe ground. I could not have endured working in the pandemic as a student without the care of my professors. Dr. Eric Domyan was a huge help in helping me feel confident in the ER and in the classroom.
Medical professionals are doing their job, just like everyone else. I don't feel like a hero, and I'm certainly not above anyone else. I think we all have a part to play in this pandemic. Not one industry is better than another. It takes everyone working together to run a whole society.
*UVU Magazine staffers Jay Drowns, Layton Shumway, Jay Wamsley, Anna Tibbitts, and Alex Kennington contributed to this article.